Many radiation oncology appointments can be completed effectively using the telephone or telehealth, with only a relatively small number of these requiring subsequent face-to-face appointments, a new study has found.
"In the postpandemic era, telephone/telehealth consultations may have a role in the provision of radiation oncology services," noted senior author Dr. Amy Shorthouse, a radiation oncologist at the Canberra Hospital in Garran, Canberra, Australian Capital Territory, and her colleagues. "However, careful patient selection and accounting for multiple variables would be needed to ensure effective and safe healthcare is provided."
Patients with tumor subsites that were more easily surveyed radiologically or biochemically, rather than by direct physical examination, were less likely to require subsequent face-to-face consultations following telephone/telehealth consultations, they reported in an e-poster presentation at the recent Royal Australian & New Zealand College of Radiology (RANZCR) annual scientific meeting.
The switch to telehealth
In late March 2020, the Australian government expanded the Medicare-subsided telehealth services amid the evolving COVID-19 pandemic. This was in response to a ban on all in-person healthcare with limited exceptions, so there was no choice for most patients and healthcare providers.
Faced by this situation, the researchers decided to track the percentage of telephone/telehealth consultations that resulted in subsequent face-to-face consultations during the first wave of the COVID-19 pandemic and assess the reasons for these face-to-face consultations. The first author for the project was Dr. A.J. McKean, also from the same hospital.
For the study, the researchers obtained a dataset via a deidentified report created from the department of radiation oncology's information system (ARIA) spanning a 10-week period from 23 March to 28 May 2020. From this report, demographic data were collated, including medical record numbers, each patient's date of birth and place of residence, and diagnoses (ICD-10 code). This was supplemented with clinic appointment information, including appointment types, dates, and times.
During the period, a total of 1,159 consultations were performed on 973 patients. About 60% (700) of all consultations were performed by telephone/telehealth, with less than 1% (4) of these by telehealth. The remaining 40% of consultations were conducted face-to-face.
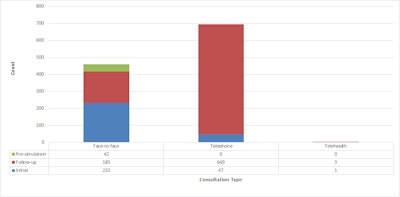 Consultation types. All figures courtesy of Dr. A.J. McKean and colleagues, presented at RANZCR annual congress.
Consultation types. All figures courtesy of Dr. A.J. McKean and colleagues, presented at RANZCR annual congress.While initial consultations were more commonly performed face-to-face than via telephone/telehealth, the majority of follow-up consultations were conducted via telephone than face-to-face.
Sixty-six (9% of all telephone/telehealth) patients required a subsequent face-to-face consultation following their telephone/telehealth consultation within the study period.
The reasons for these face-to-consultations are outlined in the figure below.
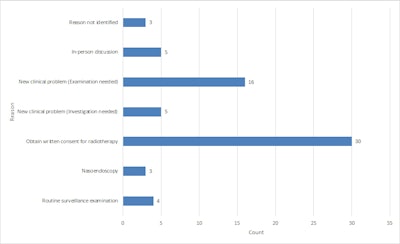 Reason for subsequent face-to-face consultation following a telephone/telehealth consultation.
Reason for subsequent face-to-face consultation following a telephone/telehealth consultation.Of the 16 patients requiring a physical examination for a new clinical problem, the primary sites of disease were breast (4), mucosal head and neck (3), skin (3), endometrium (2), oral cavity (1), rectal (1), lung (1), and prostate (1).
Also, of the five patients requiring further investigation(s), the primary sites of disease were prostate (3), mucosal head and neck (1), and benign meningeal disease (1).
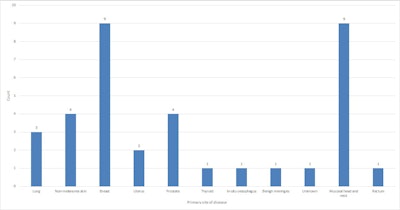 Primary site of disease (written consent excluded) of patients attending for subsequent face-to-face consultation.
Primary site of disease (written consent excluded) of patients attending for subsequent face-to-face consultation.Routine examinations were performed on three breast cancer patients and one patient with a mucosal head and neck primary, the authors wrote.
Further reflections
Interestingly, when telehealth Medicare Benefits Schedule (MBS) items were first introduced in Australia, they had to be bulk-billed (BB, i.e. no out-of-pocket costs for the patients and 85% of the government-determined scheduled fee paid to the doctor). The Australian Medical Association lobbied against this. The government wanted to stop telehealth, but finally continued it (not indefinitely) and removed the BB requirement.
Looking to the future, it will be useful to know if the telehealth continued once the first wave of the pandemic passed in Canberra and also what the patients thought of it. In the U.K., for instance, concerns have been raised by coroners over missed diagnoses when consultations were remote. Also, some oncology patients have shown a preference for in-person consultations, and the potential downside of telehealth is that it disconnects doctors, including radiologists, from patients and referrers and commoditizes radiology.