The European Society of Thoracic Imaging (ESTI) and the European Society of Radiology (ESR) have unveiled a new document on the role of imaging in the long-term follow-up of COVID-19 patients. Written by 14 leading chest radiologists, the aim is to define which patients may benefit from imaging and what modalities and protocols should be used.
The group has sought to provide insights into features encountered on CT scans. Potential pitfalls and areas for future review and research are also included in the report, which was published on 29 October by European Radiology.
"Imaging follow-up should be performed after a delay to allow resolution of the reversible inflammatory process in symptomatic patients," noted first author Dr. Katharina Martini, senior physician at Zurich University Hospital, and her co-authors.
"Unenhanced low-dose CT performed supinely should be sufficient in the vast majority of COVID-19 patients for follow-up. Expiratory CT and single- or dual-energy contrast-enhanced studies should only be performed on selected patients, after clinical and functional evaluation," they stated.
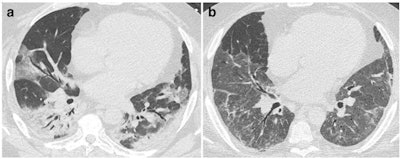 CT features at baseline and at discharge in a 52-year-old man who developed severe COVID-19 pneumonia (intubation, extracorporeal membrane oxygenation, 45 days in intensive care unit). a: Baseline CT shows bilateral consolidation and ground glass opacities (GGOs) with peripheral and peribronchovascular distribution. b: 2-month CT follow-up demonstrates the complete resolution of consolidation, with residual parenchymal bands bilaterally, while GGOs appear more extensive ("tinted sign") in the lower lobes, lingula, and right middle lobe. Note the improved expansion of the left lung in b. Figures courtesy of Dr. Katharina Martini et al. and European Radiology.
CT features at baseline and at discharge in a 52-year-old man who developed severe COVID-19 pneumonia (intubation, extracorporeal membrane oxygenation, 45 days in intensive care unit). a: Baseline CT shows bilateral consolidation and ground glass opacities (GGOs) with peripheral and peribronchovascular distribution. b: 2-month CT follow-up demonstrates the complete resolution of consolidation, with residual parenchymal bands bilaterally, while GGOs appear more extensive ("tinted sign") in the lower lobes, lingula, and right middle lobe. Note the improved expansion of the left lung in b. Figures courtesy of Dr. Katharina Martini et al. and European Radiology.The team's key points are as follows:
- Post-COVID-19 pneumonia changes are mainly consistent with prior organizing pneumonia and are likely to disappear within 12 months of recovery from the acute infection in the majority of patients.
- At present, with the longest series of follow-up examinations reported not exceeding 12 months, the development of persistent or progressive fibrosis in at least some individuals cannot yet be excluded.
- Residual ground glass opacification may be associated with persisting bronchial dilatation and distortion and might be termed "fibrotic-like changes" probably consistent with prior organizing pneumonia.
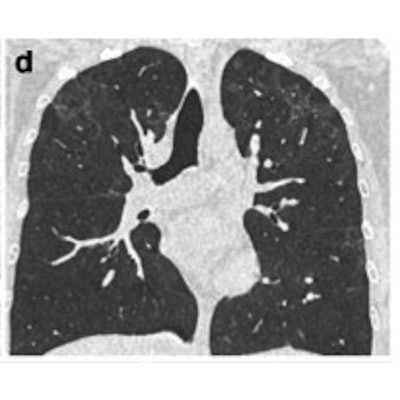
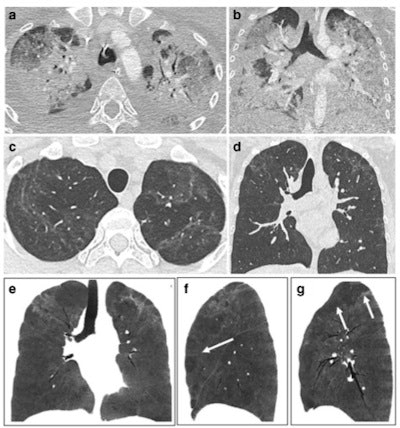 CT features at baseline, and one-year follow-up, in a 30-year-old woman who developed severe COVID-19 pneumonia (intubation, 40 days in intensive care unit). a,b: Baseline CT showing extensive ground glass opacities (GGOs) and consolidation. c–g: 1-year CT follow-up. Residual GGO, with a linear shape, is mainly seen in the upper lung, suggestive of organizing pneumonia at a late phase. There is no bronchial dilatation, signs of architectural distortion, or honeycombing, as confirmed by minimum intensity projections (minIP) (e, f, g). The sagittal minIP reformations (f, g) demonstrate plurilobular areas of decreased attenuation (arrows). This mosaic attenuation pattern might be due to either residual small airway disease or peripheral vascular obstruction. Decreased diffusing capacity (DLCO) at one year was 64%.
CT features at baseline, and one-year follow-up, in a 30-year-old woman who developed severe COVID-19 pneumonia (intubation, 40 days in intensive care unit). a,b: Baseline CT showing extensive ground glass opacities (GGOs) and consolidation. c–g: 1-year CT follow-up. Residual GGO, with a linear shape, is mainly seen in the upper lung, suggestive of organizing pneumonia at a late phase. There is no bronchial dilatation, signs of architectural distortion, or honeycombing, as confirmed by minimum intensity projections (minIP) (e, f, g). The sagittal minIP reformations (f, g) demonstrate plurilobular areas of decreased attenuation (arrows). This mosaic attenuation pattern might be due to either residual small airway disease or peripheral vascular obstruction. Decreased diffusing capacity (DLCO) at one year was 64%.The report devotes a section to the role of CT pulmonary angiography (CTPA) and dual-energy CT (DECT). DECT enables assessment of pulmonary perfusion and the detection of capillary microvascular thrombosis.
"If validated in larger series, DECT might be used in patients with persisting abnormal gas exchange despite apparent normalization of lung parenchyma on CT," the authors wrote. "To date, there is no evidence in the literature that macrovascular disease plays a role in long COVID or post-COVID syndrome."
It is unclear if there are still peripheral perfusion deficits in the late follow-up, so CTPA is only suggested if there is further evidence of pulmonary embolism following the general consideration of pretest probability and D-dimers, especially if supplementary oxygen is needed in patients with limited disease extension. Also, CTPA can be considered in the follow-up of patients who had PE in the acute phase of the disease, they noted.
Clinical aspects in the follow-up of COVID-19 patients are to be released in a statement (currently under review) from the European Respiratory Society (ERS), according to Martini and colleagues.