Which modality is the most appropriate choice to diagnose suspected local recurrence of head and neck squamous cell carcinoma (HNSCC)? Dutch researchers chose FDG-PET/CT over MRI in a study published in the February issue of the European Journal of Radiology.
The modalities achieved similar diagnostic accuracy, and MRI was superior in specificity, but FDG-PET/CT's higher sensitivity was the determining factor in deciding how best to evaluate patients after radiotherapy with or without chemotherapy.
"During follow-up after chemoradiation, early detection of residual or recurrent disease is one of the main objectives, as salvage surgery might still be a curative option," wrote lead author Dr. Juliette Driessen and colleagues from the University Medical Center Utrecht (EJR, February 2019, Vol. 111, pp. 62-67). "In this scenario, a high sensitivity is the most important feature of an imaging modality."
Detection challenge
Clinicians routinely follow up a patient's cancer treatment to look for signs of possible recurrences, especially if related symptoms occur. Early detection can reduce the chance of patients having to undergo salvage surgery and could improve their survival and quality of life. The challenge is differentiating between actual local recurrence and postradiation effects, such as fibrosis, edema, and inflammation, which can mimic tumor recurrence, the authors noted.
FDG-PET/CT has been shown to provide high negative predictive value for local recurrence, but the hybrid modality also could report false-positive results due to FDG uptake in areas of inflammation and tissue changes after radiation therapy. On the other hand, diffusion-weighted MR imaging (DWI-MRI) is known to accurately discern between malignant and benign lesions and, thus, add to the detection of local HNSCC recurrences.
To help answer the question of which modality offers the best option, the researchers compared FDG-PET/CT with DWI-MRI among patients with suspected local recurrence of HNSCC after radiotherapy with or without chemoradiation.
Prospective approach
For this prospective study, Driessen and colleagues consecutively enrolled 70 patients with a median age of 61 years (range, 42-81 years) between April 2011 and November 2014. The 51 men and 19 women were suspected of having local recurrence of laryngeal, hypopharyngeal, or oropharyngeal cancer based on new or persistent symptoms between three months and three years after completing treatment. Initial primary tumor stage ranged from 1 to 4b, while node stage ranged from 0 to N2c.
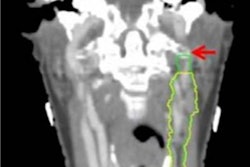
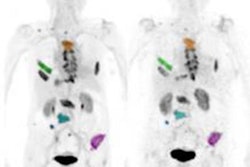
MRI scans were performed on a 3-tesla system (Intera NT, Philips Healthcare) with a dedicated head and neck coil. The protocol included transverse T1-weighted turbo spin echo (TSE) before and after gadolinium and echo-planar DWI-MRI. FDG-PET/CT imaging was performed on a whole-body scanner (Biograph mCT, Siemens Healthineers) approximately one hour after injection of 2.0 MBq/kg of FDG and after a six-hour fasting period. Median time between the MRI and FDG-PET/CT exams was one day (range, 0-31 days).
Readers of the MR images were blinded to FDG-PET/CT results, and all reviewers were blinded to the clinical outcome. They used the results of biopsy or the absence of a recurrence as the reference standard.
Regarding the modalities' performances, FDG-PET/CT detected positive local recurrence in 51 patients (73%), compared with only 32 positive local recurrent cases (46%) with DWI-MRI. Two FDG-PET/CT results were inconclusive.
In calculating diagnostic accuracy, the researchers considered inconclusive results as positive. Also, FDG-PET/CT had a similar diagnostic accuracy (72%), compared with MRI (73%) (p = 0.85). Interestingly, FDG-PET/CT's sensitivity was significantly superior to DWI-MRI (p < 0.01), but FDG-PET/CT was significantly inferior for specificity, compared with its counterpart (p < 0.01). FDG-PET/CT's sensitivity was buoyed by reporting 33 true-positive results (94%), compared with 24 true positives (68%) for DWI-MRI.
| Diagnostic accuracy of FDG-PET/CT vs. DWI-MRI | ||
| FDG-PET/CT | DWI-MRI | |
| Sensitivity | 97%* | 69% |
| Specificity | 46% | 77%* |
| PPV | 64% | 75% |
| NPV | 94% | 71% |
| Accuracy | 72% | 73% |
*Statistically significant difference.
Conversely, the rate of false-negative results was a key differentiator between the two modalities. FDG-PET/CT had only one false positive (3%) among 35 cases, compared with 11 false positives (31%) for MRI.
"False-negative results of a selection strategy can have tremendous effects," Driessen and colleagues wrote. "They will cause delay in detection of recurrences, which will potentially influence the chance of successful salvage surgery. Therefore, we consider FDG-PET/CT to be superior to MRI, including diffusion-weighted sequences, in the early diagnosis of recurrence of HNSCC after chemoradiotherapy."
Better together?
Given the capabilities of both modalities, how would combining them improve local recurrence detection for HNSCC? Perhaps somewhat surprisingly, the results were rather limited. Sensitivity increased to 100%, but the combined modalities still erroneously reported 20 patients with local recurrence, which was one patient more than FDG-PET/CT alone.
"It is debatable whether the difference in early detection of recurring disease in one patient at the cost of one extra patient with an unnecessary biopsy justifies a combined use of FDG-PET and MRI," the researchers concluded.