The U.K. Royal College of Radiologists (RCR) has released new free guidance designed to improve radiological recognition and actionable reporting of osteoporotic vertebral fragility fractures (VFFs).
"VFFs are common and are frequently present on imaging, but are rarely reported. This missed opportunity has an impact not only on patient morbidity and quality of life but vertebral fractures themselves are associated with an increase in age-adjusted mortality and are a predictor of future osteoporotic fractures," the authors noted.
Several factors contribute to underdiagnosis following imaging, including the failure of radiologists to consistently review spinal components of imaging, lack of awareness of the importance of early diagnosis of VFFs and use of ambiguous reporting terminology (e.g., "loss of height" or "wedging"), immature or underdeveloped departmental RIS and alert processes inhibiting rapid dissemination of reports, and inadequate onward referral systems (in particular fracture liaison services), they wrote.
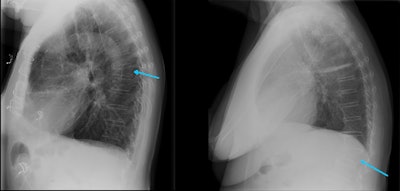 Radiologists and reporting radiographers are well-placed to diagnose VFFs on any modality that can provide images of the spine, including x-ray. All images courtesy of Dr. Anagha Parkar, Bergen, Norway.
Radiologists and reporting radiographers are well-placed to diagnose VFFs on any modality that can provide images of the spine, including x-ray. All images courtesy of Dr. Anagha Parkar, Bergen, Norway.These are the 12 key points in the RCR guidance:
- Appoint a radiology osteoporosis lead to support development, delivery, and audit of policy and protocol in the identification and reporting of fragility fractures, including VFFs, and to act as part of a multidisciplinary team (within a local fracture liaison service [FLS] if available).
- Agree local policies for the opportunistic reporting of VFFs from imaging that includes the spine.
- Agree local policy for adopting a consistent approach to the identification and reporting of VFFs.
- Implement a policy of automatic sagittal spinal reformatting and display and storage on PACS for cross-sectional imaging studies that include the spine.
- Consider a policy for template reporting of cross-sectional imaging studies that include the spine to cover bone integrity, presence of VFF, level, and grade/severity.
- Implement a policy for standardized use of terminology for VFFs -- using the term "vertebral fracture."
- Implement routine audit processes around identification and reporting of VFFs.
- Agree local policy for onward alerting of referrers or referral to fracture prevention pathways.
- Agree service-level agreements (SLAs) with teleradiology contractors to adopt and adhere to VFF-reporting policies.
- Consider the use of standard phrases or short codes to create actionable reports or alerts to referrers.
- Where artificial intelligence (AI) technology is implemented to actively screen cross-sectional imaging, agree processes and policy for radiological correlation and alert reporting.
- Discuss and agree the use of alerts, report content, and automization, and clarify onward referral pathways. Clinical engagement is beneficial. Severe or multiple VFFs or cases with canal compromise will warrant urgent clinical evaluation.
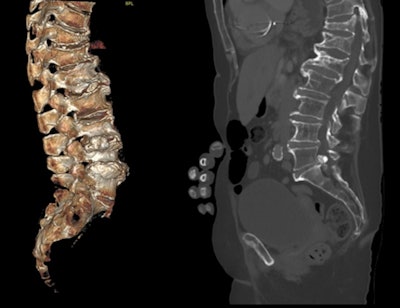 With body CT scanning, performing sagittal bone reformats of the spine does not require additional scan times or radiation dose, nor does it require significant additional storage space. To increase VFF detection on body CT, sagittal reconstruction of the spine using bone windows should be sent routinely to PACS for storage and display.
With body CT scanning, performing sagittal bone reformats of the spine does not require additional scan times or radiation dose, nor does it require significant additional storage space. To increase VFF detection on body CT, sagittal reconstruction of the spine using bone windows should be sent routinely to PACS for storage and display."Emerging AI technology and algorithms have scope to support the identification of VFFs through routine scrutiny of cross-sectional imaging via PACS and the creation of 'alert lists' of those patients with suspected VFFs. Radiological interpretation may still be required to verify absence or presence of AI-identified VFFs since this technology is currently limited in differentiating between VFFs and non-fracture deformities such as Scheuermann's disease or Schmorl's nodes," the authors stated.
While AI technology may identify patients with VFFs and append this data to PACS, processes must be developed by individual services to ensure radiological actionable reports and alerts are issued for these patients to access appropriate onward assessment and care, they added.
This guidance has been endorsed by the British Society of Skeletal Radiologists, the Royal College of Physicians, and the Royal Osteoporosis Society. It is applicable to all individuals who report imaging that may incorporate the spine, including radiologists reporting onsite and offsite (including teleradiology) and reporting radiographers, according to the authors.
The 12-page document can be downloaded free of charge from the RCR website.