One-view digital breast tomosynthesis (DBT) is not statistically inferior to two-view digital mammography (DM) or two-view DM plus two-view DBT, Dutch researchers have found. Furthermore, one-view DBT could be sufficient for experienced readers, they added.
The research team, led by Dr. Alejandro Rodriguez-Ruiz from the radiology and nuclear medicine department at Radboud University Medical Center in Nijmegen, the Netherlands, compared all three protocols and found one-view DBT performs similarly to standard protocols, especially for experienced readers.
"Experience with single-view DBT interpretation might change the operating point of radiologists, making their sensitivity/specificity performance in a screening scenario equivalent to that of two-view DM plus two-view DBT," the study authors wrote (European Radiology, 11 December 2017). "Therefore, with a wide-angle system and appropriate training, MLO [mediolateral oblique] view-only DBT might be feasible for breast cancer screening."
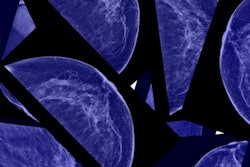
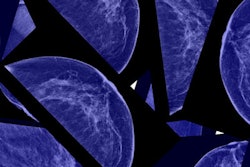
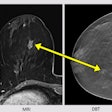
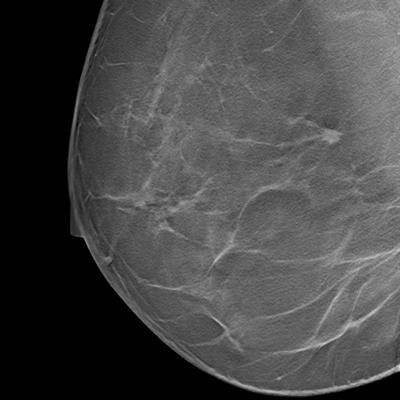
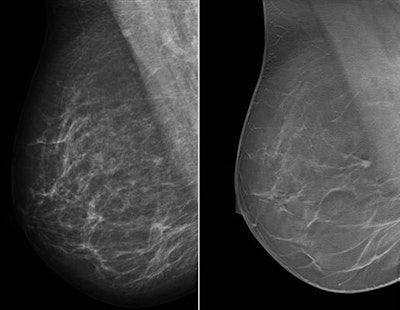 Single-view right MLO mammogram and corresponding DBT slice show the improvement in cancer visibility that can be achieved with tomosynthesis. There is a small cancer visible in the DBT slice just before the pectoral. The lesion is barely recognizable on the concurrent mammogram. All images courtesy of study co-author Dr. Ritse Mann.
Single-view right MLO mammogram and corresponding DBT slice show the improvement in cancer visibility that can be achieved with tomosynthesis. There is a small cancer visible in the DBT slice just before the pectoral. The lesion is barely recognizable on the concurrent mammogram. All images courtesy of study co-author Dr. Ritse Mann.Wide-angle DBT
More and more, radiologists are looking to DBT when it comes to breast cancer screening. Research continues to mount regarding the modality's usefulness in the real world, particularly when paired with synthesized 2D mammography, or a 2D mammogram culled from DBT slices.
However, this results in increased reading time. Does cutting down to only an MLO view versus an MLO and craniocaudal (CC) view make a difference? That's precisely what Rodriguez-Ruiz and colleagues sought to find out.
They focused specifically on wide-scan angle DBT systems -- those acquiring the projection images over an angular range of 40° to 50° -- because new studies indicate DBT is not inferior to DM even for wide-scan angle DBT systems, eliciting the possibility of using DBT as a standalone modality. Wide-scan angle DBT systems yield improved depth information that better exploits the 3D advantage of DBT over DM, possibly making two breast views unnecessary.
Preliminary studies have shown using only the MLO view of a wide-scan angle DBT system resulted in better breast cancer detection compared with two-view DM. In this study by Rodriguez-Ruiz and colleagues, they further explored the potential of one-view DBT for breast cancer detection in screening by performing a retrospective reader study with an enriched case dataset.
They compared the clinical performance of one-view DBT with three other protocols: one-view DBT (MLO) plus one-view DM (CC), two-view DM, and two-view DM plus two-view DBT. They also evaluated the strengths of one-view DBT as a standalone technique stratified by lesion type, breast density, and radiologist experience.
The researchers used DM and DBT (Mammomat Inspiration, Siemens Healthineers) images from 181 women imaged between December 2014 and December 2015 who were recalled from screening or had a clinical indication for imaging. Within the cohort, 76 patients had malignant lesions and 50 had benign lesions, all verified by histopathology. Four patients had multiple lesions. In total, 130 lesions were diagnosed with histopathological proof (79 malignant, 51 benign). The remaining 55 patient cases were interpreted as normal.
For each patient, two-view DM and two-view DBT (CC and MLO) were obtained. Four different unilateral image sets resembling four different imaging protocols were created for each patient: one-view DBT (MLO), one-view DBT (MLO) plus one-view DM (CC), two-view DM, and two-view DM plus two-view DBT.
The researchers found no difference between one-view DBT and the other modalities either for sensitivity (p = 0.536) or specificity (p = 0.553). However, they spotted differences among the six readers -- for the group of radiologists experienced with one-view DBT, there was no statistically significant difference either in sensitivity (p = 0.776) or specificity (p = 0.482) when compared with the other protocols.
For the inexperienced group, sensitivity increased for all the other protocols with respect to one-view DBT (only significant for two-view DM, from 69% to 79%), while specificity was slightly higher for one-view DBT with respect to the other protocols.
Results are listed in the table below.
| Sensitivity & specificity of one-view DBT compared with other protocols | ||||
| One-view DBT | One-view DBT + one-view DM |
Two-view DBT + two-view DM |
Two-view DM | |
| Total sensitivity | 72% | 75% | 76% | 76% |
| Total specificity | 74% | 72% | 73% | 76% |
The researchers also found the mean glandular dose for one-view DBT equaled that of two-view DM (2.41 ± 0.87 mGy versus 2.41 ± 0.83 mGy). The mean dose for one-view DBT plus one-view DM was 3.62 ± 1.25 mGy, and for two-view-DBT plus two-view DM, it was 7.23 ± 2.49 mGy.
DBT also performed as well as the other protocols for detection calcifications, suggesting that DBT is not inferior for detecting calcifications even with a wide-angle DBT system, they added.
"Logically, the use of one-view DBT is very beneficial for the women undergoing screening, not only for the radiologist, as it requires only a single compression per breast (rather than the current two)," corresponding author Dr. Ioannis Sechopoulos told AuntMinnieEurope.com. "In addition, the implementation of DBT for screening is challenging due to the increase in reading time (about double for DBT compared to mammography). Reading only one view would reduce the reading time substantially, allowing DBT screening in perhaps the same time as is currently necessary for reading two-view mammography."
They found one-view DBT took on average 25% longer to read than two-view DM, although reading times were equivalent for half of the observers. It is also possible that longer DBT loading times influenced reading times.
"Additional training of radiologists on reading DBT, the inclusion of synthesized mammograms, and computer-aided detection systems might aid speeding the reading of DBT," Rodriguez-Ruiz and colleagues wrote.
Especially as inexperienced readers gain more familiarity with DBT, screening with one-view DBT becomes more feasible, they added. They pointed out that the results apply to wide-angle DBT systems and may not remain true for narrow-angle ones.
In terms of future research, the researchers plan to investigate other strategies and methods to reduce the reading time of DBT.
"In addition, given the recent developments in artificial intelligence algorithms, the next step is to evaluate whether the readers can improve their performance with one-view DBT by using a computer system as decision support," Sechopoulos told AuntMinnieEurope.com. "Eventually, it would also be valuable to compare single-reading with decision support versus double-reading of one-view DBT, to optimize the implementation of DBT in screening practice."