
Artificial intelligence (AI) coupled with advanced functional imaging will produce more specific diagnoses in a wide range of psychiatric disorders that are notoriously difficult to diagnose, and ultimately technology can lead to more personalized therapy, according to French experts.
Dr. Sidney Krystal, a neuroradiologist at the Rothschild Foundation Hospital in Paris and CHU Lille, noted that psychiatric pathologies are the most frequent of all pathologies, ahead of cancer and cardiovascular disease, affecting one person in four. Seven million French people have depression, and 20% of the population will experience at least one episode of depression in their lives. Furthermore, 1.6 million have bipolar disorder, accounting for more than 2% of the population, and 650,000 are on the autism spectrum.
Despite widespread incidence, particularly in adolescents, diagnosis is tricky, Krystal told attendees recently at a special session during the French national congress, Journées Francophones de Radiologie (JFR).
"Psychiatric pathologies are serious and a major cause of mortality -- if not directly by suicide, then from other causal factors such as addiction, incorrect hygiene and diet and self-neglect, all reducing life expectancy," he noted. "Early diagnosis leads to timely patient treatment and management and better outcomes."
 Pathologies induced by taking toxic substances, such as methotrexate toxicity. Neurotoxicity related to methotrexate can result in a range of acute and chronic leukoencephalopathies, and permanent neurological deficits may be unilateral or bilateral. Courtesy of Dr. Riyad Hanafi, CHU de Lille, and JFR 2021.
Pathologies induced by taking toxic substances, such as methotrexate toxicity. Neurotoxicity related to methotrexate can result in a range of acute and chronic leukoencephalopathies, and permanent neurological deficits may be unilateral or bilateral. Courtesy of Dr. Riyad Hanafi, CHU de Lille, and JFR 2021.The problem is that there is no reliable objective diagnostic tool, and diagnosis often relies on subjective clinical suspicion, which lacks reproducibility, he added.
Bipolar disorder
In his JFR talk, Krystal focused on bipolar illness -- a "young person's" disorder that is often first diagnosed in 15- to 19-year-olds. Diagnosis tends to be based on successive episodes of depression and mania, associated with other problems such as addiction and anxiety, and potentially may be confused with other personality disorders and schizophrenia.
The specific treatment for bipolar disorder is lithium salt, but the therapeutics action mechanism remains poorly understood, he said.
"A better understanding of the pathophysiology of this disease and the mechanism of action of the treatment will make it possible to offer more appropriate management," he noted.
Autism too, affects the very young, first appearing in children between 18 and 36 months. It manifests itself in various learning disabilities and difficulty socializing as well as other symptoms such as abnormal social interaction, repetitive behavior, and unusual reaction to sensations. Autism is also associated with depression, sleep problems, and epilepsy, and timely diagnosis can obviate the onset of extra handicaps.
Psychiatric imaging research must change the current paradigm, Krystal emphasized. He is part of the NeuroSpin trial team in functional imaging for psychiatric pathologies, a project led by Prof. Josselin Houenou that aims to optimize diagnostic imaging in the management of psychiatric pathologies and mental health so as to arrive at a positive diagnosis.
This paradigm shift involved ruling out differential diagnoses. For example, 1% to 2% of psychiatric patients were diagnosed with an organic etiology such as tumors and encephalitis. Neuroradiologists had to therefore identify associated pathologies and psychiatric complications and understand how to move from these goals to positive diagnosis, prognosis, and therapy.
New biomarkers
In tandem, a goal is to confirm the diagnosis for individual patients with psychiatric pathologies with the help of AI algorithms applied to advanced imaging methods, namely in MRI.
 19-year-old patient with multinodular and vacuolated neuronal tumor (MVNT). These benign neuronal lesions have a distinct cytoarchitectural pattern that may be related to ganglion cell tumors. Courtesy of Dr. Ali Amad, CHU de Lille, and JFR 2021.
19-year-old patient with multinodular and vacuolated neuronal tumor (MVNT). These benign neuronal lesions have a distinct cytoarchitectural pattern that may be related to ganglion cell tumors. Courtesy of Dr. Ali Amad, CHU de Lille, and JFR 2021.Krystal noted that neuroradiologists must redefine pathologies through the use of objective biomarkers such as connectivity rather than through clinical suspicion, understand the morphological imaging signs of these pathologies such as cortical atrophy and white-matter abnormalities, and predict the evolution of psychiatric problems and treatment response using AI methods for personalized management of the patient.
At the moment, psychiatric imaging research is focusing on resting-state functional MRI, where blood oxygenation level-dependent (BOLD) signal is followed over time to evaluate regional interactions in the brain. This signal modifies when an area of the brain activates.
By analyzing the signal in each section of the brain, radiologists can build a connectivity matrix that can be studied for different information, he continued.
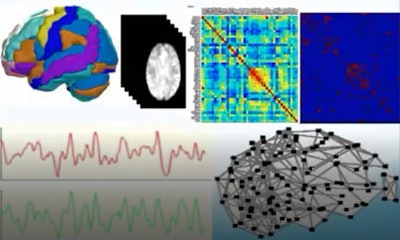 Resting-state functional MRI is acquired in the absence of a stimulus or a task. Courtesy of Dr. Sidney Krystal and JFR 2021.
Resting-state functional MRI is acquired in the absence of a stimulus or a task. Courtesy of Dr. Sidney Krystal and JFR 2021.Looking at a patient's functional brain network, neuroradiologists can define connectivity -- or lack of it -- between brain regions, which provides evidence of disorders such as bipolarism. For example, in bipolar patients, the part of the brain that controls emotion will remain active during other tasks when it would normally deactivate.
Such maps show hyperactivity between the amygdala, which triggers emotions, and the medial prefrontal cortex, which regulates them. These specific anomalies in psychiatric pathologies can be seen and measured through imaging, as can reduction in anomalies during treatment. Efficacy of treatment can therefore also be studied.
Future patient management
Krystal noted that pilot studies in bipolar patients were now looking at the connectivity profile of the amygdala. When the amygdala is strongly connected to the hippocampus, it is thought that this connectivity between the two is indicative of depression, but when the amygdala is strongly connected to the nucleus accumbens, the patient conversely is thought to be in a manic phase.
He also highlighted how the application of AI -- particularly unsupervised machine learning using biomarkers such as connectivity -- may lead to better patient management: Type 1 and 2 bipolar disorder has no genetic cause or physiopathological basis and no specific treatment.
Supervised machine learning with functional MRI may consolidate the classification of patients, allowing doctors to pronounce the probability of bipolarism. Nonsupervised machine learning, on the other hand, will redefine classifications and create more homogenous groups of patients. For example, type A patients may have one sort of connectivity, while type B will have another sort.
For patients on the autism spectrum, functional connectivity anomalies, notably in the cerebellum, may also lead to a redefinition of categories within this large and varied cohort of patients.
"Artificial intelligence will find and define homogeneous subgroups of patients to whom doctors can propose specific treatments," Krystal said.



















