Interactively employing computer-aided detection (CAD) technology while reading mammograms may lead to increased detection of breast masses, according to research from Radboud University Nijmegen Medical Centre in Nijmegen, Netherlands.
"Readers performed better with interactive CAD compared to unaided reading," said Nico Karssemeijer, Ph.D. He presented the study team's findings at the 2008 RSNA meeting in Chicago.
Many radiologists have little confidence in CAD due to the technology's poor specificity in breast masses, Karssemeijer said. Current CAD systems only address the problem of perception errors; however, misinterpretation is a much more common cause of missing breast cancer in screening programs than perceptual oversights, he said.
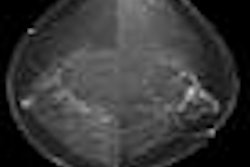
Believing that providing readers access to CAD mark probabilities could be extremely valuable, the Radboud researchers sought to study the effectiveness of an interactive use of CAD. In this approach, readers can probe regions for CAD information during the reading process to improve their decision making, rather than viewing traditional CAD marks after the case is read, Karssemeijer said.
A dedicated mammography workstation and ImageChecker v8.0 CAD software (Hologic, Bedford, MA) were used in the study. If available, the CAD region was displayed with a color-coded boundary, ranging from red for regions with a high malignancy rating to green for regions with low malignancy ratings, he said. The study team set the number of CAD regions that could be activated to an average of two false positives per image.
The study team then evaluated the approach using an observer study with seven readers (two certified mammographers and five nonradiologists with mammography experience). The radiologists each read 60 cases (20 with cancer), while the nonradiologists read 120 cases (40 with cancer). Nonradiologists were trained with a separate series of 60 cases.
All of the cancer cases selected for the study had been missed at screening and were retrospectively identified as visible, according to the researchers. The study team excluded cases that only had microcalcifications. True positives were defined as cancers correctly localized.
The readers read each mammogram both with and without CAD in two different sessions, and they reported localized findings with malignancy ratings per finding scored on a continuous scale, Karssemeijer said. The researchers calculated sensitivity based on correct cancer localization fraction, which was computed for each reader as a function of the fraction of normal cases that would be recalled based on the malignancy ratings.
Using an interval of negative recalls less than 10%, mean sensitivity was 27.1% in the sessions without CAD and 36.9% in the sessions with CAD, he said. The improved performance was statistically significant (p < 0.01).
The mean sensitivity of the two radiologists was 27.4% without CAD and 32.7% with CAD.
"Results of reading with CAD were comparable to independent combination of the reader scores with CAD," he said. "Nonradiologists had a lot more benefit [from CAD], but they also had a lot more training with the system."
Readers probed an average of 13.6 locations per case for CAD information, according to the researchers. The average reading time was 105 seconds per case in the sessions without CAD, compared with 104 seconds per case when CAD was used.
By Erik L. Ridley
AuntMinnie.com staff writer
December 22, 2008
Related Reading
New mammo CAD approach lowers false positives, December 2, 2008
NEJM study finds single reading with mammo CAD matches double reading, October 2, 2008
Study finds that CAD improves mammography's sensitivity, February 13, 2008
Mammo CAD results show reproducibility in serial exams, January 10, 2008
UnitedHealthcare postpones CAD decision, November 27, 2007
Copyright © 2008 AuntMinnie.com