Early recognition of the CT signs of hypovolemic shock complex by alert and well-trained radiologists can facilitate identification of acutely unwell patients and prompt treatment and improved patient outcomes, according to a leading group of Irish researchers.
"While visceral injuries and abnormalities are often readily identified via CT, hypovolemic shock is infrequently encountered and often not appreciated," noted Dr. Stephen Power, a radiologist at Cork University Hospital, and colleagues, who think it's important to bear in mind how CT findings can allow correlation of imaging studies to the pathophysiological response to hypovolemic shock.
The initial description of hypoperfusion complex was in children, they explained in an RSNA 2017 e-poster. The abdominal CT findings described were associated with severe injury and poor outcome, and they reflected a serious hemodynamic instability in the affected children. While these constellations of findings are typically described after major trauma, there is an association between the "shock bowel" (and other CT signs of hypovolemia) and conditions causing hypovolemic shock other than major trauma, the authors pointed out.
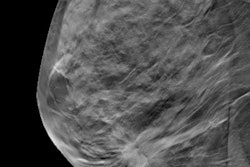
 CT image depicts the "inferior vena cava halo sign" with a thin rim of fluid surrounding the inferior vena cava in a fluid-resuscitated patient. Image courtesy of Dr. Stephen Power.
CT image depicts the "inferior vena cava halo sign" with a thin rim of fluid surrounding the inferior vena cava in a fluid-resuscitated patient. Image courtesy of Dr. Stephen Power.Inferior vena cava (IVC) flattening is likely to represent overall circulatory failure in hypotensive patients, they continued. It is defined as an anterior-posterior diameter of less than 9 mm at three levels: within the intrahepatic portion of the IVC, at the level of the renal arteries, and 2 cm below the level of the renal arteries.
Look out for halo sign
The so-called IVC halo sign refers to accumulation of extracellular fluid (HU < 20) around a collapsed IVC.
"It is present in up to 80% of hypovolemic patients, and occurs due to loss of precapillary arteriolar sphincter tone with accumulation of fluid surrounding the IVC," Power and colleagues wrote. "While periportal edema is commonly seen in biliary cirrhosis or hepatitis, it can rarely be encountered in patients following vigorous intravenous fluid resuscitation."
As for the small caliber aorta, narrowing of the anteroposterior (AP) diameter of the abdominal aorta can occur in response to hypovolemia. This results from an intense sympathetic response to decreased circulating fluid volume, and is defined as an AP aortic measurement of less than 13 mm at 2 cm above, at, and 2 cm below the origin of the renal artery, they pointed out.
During hypovolemic states, the body redirects blood toward the central organs required for survival, but an auto-regulatory process preserves bloodflow to superficial intestinal mucosa to prevent ischemia, resulting in hyperenhancement. The HU of this enhancing mucosa should be greater than that of the adjacent psoas muscle.
"Altered permeability of the intestinal wall causes leakage across the mucosa, resulting in third spacing and mucosal edema/thickening. This also causes accumulation of contrast in the bowel wall, which further accentuates the mucosal hyperenhancement," the Cork group explained. "In the post-trauma patient, this sign should not be confused with that of traumatic bowel injury."
Also, peripancreatic fluid is observed in patients with hypovolemia and pancreatitis. Peripancreatic edema can occur in up to 40% of patients with hypovolemic shock, and this is believed to relate to loss of intravascular fluid and protein with fluid moving into the interstitial space due to increased capillary membrane permeability, they added.
Other visceral manifestations
The spleen appears to be the organ most susceptible to hypovolemic shock, with hypovolemic patients demonstrating significantly reduced splenic enhancement. This hypoenhancement is believed to be secondary to hypoperfusion as the splenic artery does not possess an autoregulatory mechanism, according to the authors.
In hypovolemia cases, there is acute activation of the renin-angiotensin system. This causes a dramatic increase in resistance of the efferent renal arteriole, and results in an intense, prolonged cortical renal enhancement.
While different opinions exist among experts about the sensitivity of increased adrenal enhancement, the adrenal gland often demonstrates enhancement, which is higher than that of the surrounding vasculature, they continued.
"It can be reported when the density of the adrenal gland is greater than that of the adjacent IVC," they stated. "It is postulated to result from increased circulating contrast concentrations in situations of reduced intravascular blood volume."
Heterogeneous hepatic parenchymal enhancement pattern of the liver in shocked patients is variable, and heterogeneous enhancement is seen in a small percentage of hypovolemic patients. Preferential vasoconstriction of splenic and mesenteric veins can result in decreased portal blood flow, but these findings should not be confused with hepatic steatosis or transient hepatic attenuation differences, Power and colleagues concluded.