
Radiology in Ireland is set to come under close scrutiny at ECR 2023. Ahead of the congress, we spoke with ESR President Prof. Adrian Brady from Cork about his own career, the lessons learned from the devastating 2021 cyberattack, and the challenges facing the profession in Ireland.
Q: Can you tell us about your hospital and department?
A: Since 1995, most of my consultant career has been spent in the Mercy University Hospital in Cork, an institution founded in 1857 by the Sisters of Mercy to care for the poor of the city. Since then, the hospital has grown substantially, and it is one of two large public general hospitals in Cork, with extremely busy emergency and elective services, as well as a high level of tertiary expertise in many specialties.
 "The Mercy" is a 347-bed acute general hospital located in the middle of Cork, alongside the River Lee. It employs over 1,200 staff and treats more than 100,000 patients each year. All images courtesy of Prof. Adrian Brady.
"The Mercy" is a 347-bed acute general hospital located in the middle of Cork, alongside the River Lee. It employs over 1,200 staff and treats more than 100,000 patients each year. All images courtesy of Prof. Adrian Brady.My career has spanned a tripling of radiology departmental staff -- but it's still not enough! -- and a huge increase in workload and demand for our services. The Mercy is part of the academic hospital group affiliated with University College Cork (UCC), where I am a clinical professor in radiology. UCC has a large medical school, with undergraduate and graduate-entry streams, and it also hosts only the second school of radiography in Ireland. The current president of the European Federation of Radiographer Societies, Andrew England, PhD, is a senior lecturer in this school.
Q: What are your own specialist areas of clinical interest?
A: I'm an interventional radiologist. The healthcare system in Ireland is structured in such a way that most radiologists only practise in their subspecialty area of interest part of the time, and also have general radiology commitments. Subspecialization has become increasingly a feature of our work, but radiologist numbers don't yet support exclusive subspecialist practice. Thus, I also report lots of plain radiographs and cross-sectional imaging studies in most body areas, and even some nuclear medicine. One of the advantages of this system is that we have the opportunity to remain engaged in more general areas of radiology outside of our particular subspecialties.
A particular interest of mine for over 20 years has been hereditary hemorrhagic telangiectasia (HHT), an inherited disease characterized by abnormal blood vessels in multiple body systems and organs. We run the national referral centre for HHT in Ireland in our hospital, and I've developed an expertise in management of pulmonary arteriovenous malformations (PAVMs) in these patients.
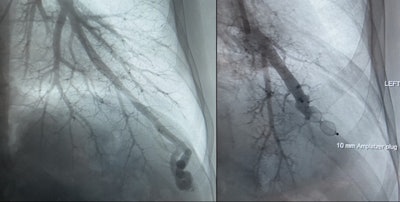 In this HHT patient treated at the Mercy University Hospital, a pulmonary AVM was diagnosed on angiography. Left image: before embolization procedure. Right image: after embolization.
In this HHT patient treated at the Mercy University Hospital, a pulmonary AVM was diagnosed on angiography. Left image: before embolization procedure. Right image: after embolization.The techniques required to embolize PAVMs have particular nuances that make them fundamentally different from some other vascular malformations, and there are very specific considerations that must be borne in mind when screening HHT patients for PAVMs, and when treating and following them up. Being intimately involved in the care of this group of patients has been hugely rewarding and fulfilling.
Q: Have you worked as a radiologist overseas?
A: I did my registrar training, or residency, in radiology at the Mater Hospital in Dublin, and then moved to Hamilton, Ontario, Canada, to pursue a fellowship in abdominal and interventional radiology. The department in McMaster University Medical Center was then led by Dr. Giles Stevenson, a giant of abdominal radiology, and a man who influenced my career in many positive ways (and whom I'm proud to call a friend).
 Shoveling snow was one of the many life skills Brady learned during his time in Canada in the 1990s.
Shoveling snow was one of the many life skills Brady learned during his time in Canada in the 1990s.After that, I moved to a staff radiologist job in the Wellesley Hospital in Toronto, which gave me a wonderful opportunity to develop my skills, especially in interventional radiology, and to gain experience at consultant level. After three great years in the Wellesley, I moved to the Mercy, where I've spent the remainder of my clinical career.
The Irish training system for most specialties encourages senior trainees to work abroad for a time period, in fellowship and staff roles, before returning to consultant positions in Ireland. I firmly believe that this way of training our most senior doctors is hugely beneficial to our healthcare system. It ensures a constant stream of highly trained and competent consultants, bringing the best of what's new and at the cutting edge of medicine from elsewhere back to our patients.
Q: Is Ireland experiencing the same sort of workforce issues and skills shortages as the U.K.?
A: Unfortunately, our staffing numbers in radiology in Ireland are even lower than those in the U.K., per head of population, and very substantially below those of most larger European countries.
The benefits of being able to obtain training abroad ensure a very high quality of healthcare delivery in Ireland, but the problem we have is with the quantity. We have fewer than 300 consultant radiologist posts in the public healthcare system, for a population of five million. This, along with a shortage of equipment and infrastructure, means that we are constantly in "emergency" mode, trying to cope with demand for services that routinely exceeds the capacity to supply. Our staffing numbers are determined and constrained by central governmental funding, and obtaining the funds to permit an increase in posts is a difficult and very slow process.
Given the growing and ageing population, our healthcare infrastructure needs massive expansion at all levels. Some political awareness of this seems to be developing, but the lead time to fund, educate, and train additional staff, and to build facilities, is very long. Our leaders are rightly talking about expanding access to diagnostic facilities (including radiology) at community level, but I fear it will be a long time before we catch up with many other countries in our capacity to deliver these services in a timely manner.
Q: The Faculty of Radiologists was created within the Royal College of Surgeons in Ireland (RCSI) in 1961. Why has a radiological society or college not been established as a separate entity?
A: The short answer is "numbers."
As a small country, many of our postgraduate specialty educational bodies exist under larger umbrellas, predominantly as constituent faculties of the RCSI or the Royal College of Physicians of Ireland (RCPI). Some specialties have formed independent colleges, but most find benefit in sharing resources and infrastructure in the RCSI and RCPI.
 Brady was elected dean of the Faculty of Radiologists in 2010.
Brady was elected dean of the Faculty of Radiologists in 2010.The Faculty of Radiologists operates very independently, controlling its own funding, membership, and educational and academic activities, but it benefits greatly from RCSI support and structures in many areas, not least in running a formal qualification exam, the Fellowship of the Faculty of Radiologists. I had the pleasure to serve on the board of the faculty for 11 years and as its dean from 2010 to 2012.
The faculty is not only a national society for radiology and radiation oncology. It also runs all training in both specialties in the country, defines training standards (under the aegis of the Medical Council), conducts the final qualifying exams, and determines successful completion of training. Thus, the faculty is a combination of a national society and the national training body.
Q: What lessons have been learned from the ransomware attack on the Irish healthcare system? Have you changed your own practice because of the attack?
A: That attack was devastating. In May 2021, the IT systems of the entire Irish public healthcare system were hacked, and effectively disabled. All IT elements were quickly taken offline, debugged, and slowly returned to service.
As a specialty almost entirely dependent on functioning IT infrastructure, radiology was impacted enormously. Suddenly, our PACS and RIS were unavailable. Various temporary workarounds were very rapidly adopted; e.g., in our hospital, we kept things going by reporting studies directly from modality monitors to a remote transcription service via our smartphones. In many cases, these solutions were needed for weeks or months.
The knock-on effects are still being felt. As a trivial example, I use my personal email address for all ESR business because the capability to access my hospital email remotely has never been restored since the attack, for security reasons.
Certainly, much has been learned. We're all much more security-conscious, and the layers of security monitoring of all IT information exchange have been greatly intensified. Some of this has slowed down workflows, and adaptations have been needed, including updating software to more recent versions.
At ECR 2023, we'll hear from speakers in two different sessions (including the "ESR meets Ireland" session) about the cyberattack and what has been learnt from it. Similar events could happen to any country; there's a lot we can all learn from the experiences of those who have already suffered attacks.
Editor's Note: We'll post the third interview article with Prof. Brady next week. Part three will focus on ECR 2023.











