Unilateral axillary adenopathy is a common side effect of COVID-19 vaccination, and more cases will be encountered by radiologists in future booster programs, researchers from a top London facility have reported.
"At the moment we are seeing no cases of vaccine-related axillary adenopathy because the last round of vaccines was some time ago," Dr. Adam Brown, consultant radiologist at the Royal Free Hospital, told AuntMinnieEurope.com on 28 September. "However, with another vaccine booster round planned in the U.K. for the winter, we expect to start seeing cases again."
He noted that the unanswered questions when COVID-19 vaccination started were which vaccines caused what degree of axillary adenopathy and for how long, as well as how should we manage breast patients with enlarged axillary nodes and a recent vaccine history, but the situation has changed.
What radiologists need to know
Imaging findings of reactive adenopathy are nonspecific, usually consisting of lymph-node enlargement and symmetrical cortical thickening.
"Important consideration must be given to the patient's vaccine history and relevant cancer risk factors to determine appropriate follow-up and management. Particular caution must be taken in patients with a history of breast cancer; there should be a low threshold for follow-up imaging and biopsy in such instances," Brown and his Royal Free colleagues stated in an e-poster presentation at ECR 2022.
Radiologists must be able to recognize typical appearances of benign reactive hyperplasia across multiple modalities and be aware of other ancillary imaging findings of vaccine-related unilateral axillary lymphadenopathy. They need to recognize the importance of obtaining an accurate vaccine history prior to any imaging of the axilla, especially during periods of mass vaccination and subsequent booster programs.
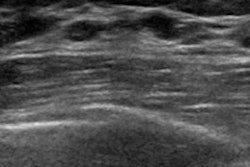
Ultrasound offers the most thorough assessment of the size and morphology of axillary lymph nodes due to its high soft-tissue resolution, according to the researchers. Sonographic changes seen in COVID-19 vaccine-related adenopathy include lymph node enlargement, a thickened cortex, and loss of the normal fatty hilum.
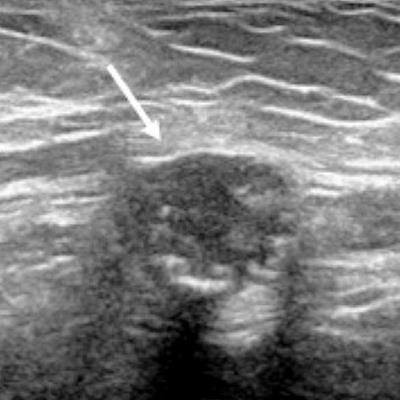
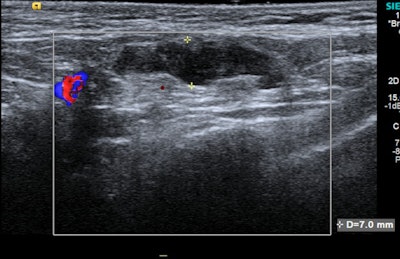 A 37-year-old woman with bilateral subpectoral implants presented to breast clinic at the Royal Free Hospital with a two-week history of palpable left axillary lump. Grey-scale ultrasound of the left axilla revealed a lymph node with cortical thickening measuring up to 7 mm. An ultrasound-guided core biopsy of the lymph node was performed, which confirmed reactive changes only. The patient had received the COVID-19 vaccine in the left arm approximately a week prior to the lymph node becoming clinically palpable. Image courtesy of Dr. Adam Brown and colleagues, presented at ECR 2022.
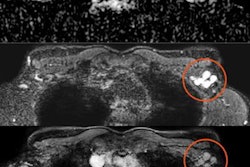
A 37-year-old woman with bilateral subpectoral implants presented to breast clinic at the Royal Free Hospital with a two-week history of palpable left axillary lump. Grey-scale ultrasound of the left axilla revealed a lymph node with cortical thickening measuring up to 7 mm. An ultrasound-guided core biopsy of the lymph node was performed, which confirmed reactive changes only. The patient had received the COVID-19 vaccine in the left arm approximately a week prior to the lymph node becoming clinically palpable. Image courtesy of Dr. Adam Brown and colleagues, presented at ECR 2022."Similarly, on CT the nodes may be enlarged with thickened cortices and possibly with surrounding fat stranding," Brown and colleagues pointed out. "A feature unique to MRI in determining vaccination as the cause of axillary adenopathy is high T2/STIR signal in the ipsilateral deltoid muscle corresponding to the injection site."
Hypermetabolic axillary nodes may also be seen on FDG-PET/CT following COVID-19 vaccination, they continued. Again, an important finding that indicates the hypermetabolic lymph node is likely to be vaccine-related is the synchronous finding of hypermetabolic inflammation in the ipsilateral deltoid muscle, corresponding to the site of injection.
At the Royal Free, all patients complete a questionnaire prior to any imaging of the axilla. This includes information such as when the patient received the vaccine, in which arm, and which type of vaccine. This aids interpretation of any axillary adenopathy detected on the subsequent scan and thereby reduces the volume of unnecessary follow-up imaging.
"We believe patients with a recent vaccination history and isolated ipsilateral axillary adenopathy should not be subject to biopsy or follow-up unless there is clinical doubt or a history of malignancy," they wrote, adding that research shows axillary lymphadenopathy can be seen for as long as 43 weeks after vaccination.
Californian experience
Another ECR 2022 presentation focused on mimickers of axillary lymphadenopathy after COVID-19 vaccination.
"In the age of increasing COVID vaccinations, it is key to differentiate reactive axillary lymphadenopathy from breast malignancy, non-breast malignancy, and benignities that share similar imaging appearances," noted Dr. Tiffany L. Chan and Prof. Cheryce Poon Fischer, from University of California, Los Angeles David Geffen School of Medicine. "This has significant implications for management, which range from return to screening to biopsy."
Women undergoing screening mammography pose a diagnostic dilemma, they explained. The U.S. Society of Breast Imaging advocates sonographic follow-up in 4-12 months for abnormal lymph nodes that are thought to be reactive, but it is crucial to recognize other oval or round structures in the axilla that may mimic the appearance of reactive axillary lymph nodes in patients who had undergone COVID vaccination, as management can greatly vary, Chan and Fischer added.
"The most common malignancy to metastasize to the axillary lymph node is primary breast malignancy and is often high in the early differential," they noted.
Nonbreast malignancies, such as soft-tissue sarcomas, are important to distinguish due to their aggressive nature and necessary treatment regimen; sarcomas represent a diverse group of malignancies that originate from the mesenchymal tissue, and as a result they can arise from any location in the body and affect all age groups, they continued.
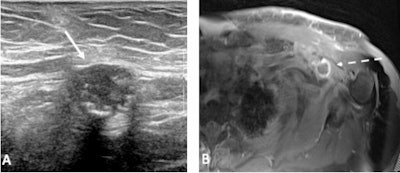 (A) Left axillary ultrasound shows a round, hypoechoic mass (solid arrow) with echogenic foci that are likely to represent calcifications. (B) Axial T1-weighted fat-suppressed postcontrast MRI reveals a rim-enhancing soft-tissue mass (dashed arrow) in the left axilla. Pathology revealed spindle cell sarcoma. Figure courtesy of Dr. Tiffany L. Chan and Prof. Cheryce Poon Fischer, presented at ECR 2022.
(A) Left axillary ultrasound shows a round, hypoechoic mass (solid arrow) with echogenic foci that are likely to represent calcifications. (B) Axial T1-weighted fat-suppressed postcontrast MRI reveals a rim-enhancing soft-tissue mass (dashed arrow) in the left axilla. Pathology revealed spindle cell sarcoma. Figure courtesy of Dr. Tiffany L. Chan and Prof. Cheryce Poon Fischer, presented at ECR 2022."There are also several benign findings that can be found in the axilla that may resemble a reactive lymph node. For example, paralabral cysts are often associated with labral tears and can cause pain, weakness, and denervation of the supraspinatus and infraspinatus muscles secondary to nerve compression. These are benign and biopsy is not recommended for confirmation," Chan and Fischer wrote.
Another important benign entity to distinguish are venous malformations, up to 40% of which are located in the extremities. Recognizing a potential vascular malformation in the axilla will prevent unnecessary biopsy, which would cause significant bleeding.
Further reading
For follow-up, Brown recommends the following article by Dr. Stacey Wolfson and colleagues at New York University Grossman School of Medicine, New York University Langone Health: "Axillary adenopathy after COVID-19 vaccine: No reason to delay screening mammogram," posted on 8 February 2022 by Radiology.
Also, you can view the Royal Free group's e-poster (co-authors Drs. S. Shah, S. Dluzewski, B. Musaddaq, A. Malhotra), as well as the Chan/Fischer ECR exhibit, on the EPOS section of the European Society of Radiology website.