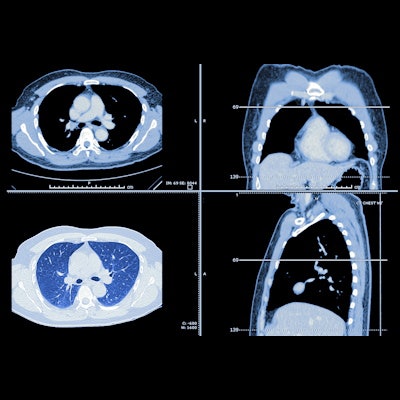
A new Dutch-led study has shown that combined low-dose CT (LDCT) screening for lung cancer, chronic obstructive pulmonary disease (COPD), and cardiovascular disease (CVD) can be cost-effective -- and it is likely to be more cost-effective than screening for lung cancer only.
In the article published online in European Radiology on 1 January, authors from the universities of Twente, Groningen, and Melbourne (Australia) explained how chest LDCT, used in lung cancer screening, can detect early stages of COPD through emphysema or air trapping evaluation, and high CVD risk based on coronary calcium scoring.
They also revealed that to be cost-effective with the same screening population and willingness-to-pay (WTP) threshold, lung cancer-only screening should cost less than 113 euros per screened individual. However, this is only an early economic evaluation, and more knowledge into the co-occurrence of these diseases is required to identify the optimal target screening population, they emphasized.
Headroom analysis
The benefits of LDCT screening of COPD and CVD are not fully clear, but the authors believe the additional screening for these diseases within a lung cancer screening program could further improve outcomes at marginal additional costs as lung cancer screening patients often have high but unrecognized CVD risk.
"To our knowledge, this study is the first to apply a headroom analysis estimating the maximum acceptable cost for a screening program," noted first author Dr. Carina Behr, a PhD candidate in health technology assessment at University of Twente, and colleagues.
"For Big-3 combination screening to be potentially cost-effective for a screening population of current and former smokers between ages 50 and 75, costs should be substantially less than 971 euros for a WTP of 20,000 euros per quality-adjusted life year (QALY) and 3,844 euros for a WTP of 80,000 euros/QALY."
Evidence from this study will help determine if combination screening of the three diseases -- collectively known as the Big-3 -- could offer an alternative to screening for lung cancer only, the authors noted. They aimed to estimate the maximum acceptable cost under optimistic circumstances per screened individual in the Netherlands for lung cancer screening and to determine the impact of additional screening for COPD, CVD, or both.
If the maximum acceptable cost is exceeded, a program is unlikely to be cost-effective, they said.
Influence of NELSON
The researchers looked at the high-risk target screening population of current and former smokers aged 50–75 in The Netherlands, corresponding to the population of the Dutch-Belgian Randomized Lung Cancer Screening (NELSON) trial.
The maximum acceptable cost per individual for implementing lung cancer screening at a WTP threshold of 20,000 euros/QALY was 113 euros. If COPD, CVD, or both were included in screening, the maximum acceptable cost increased to 230 euros, 895 euros, or 971 euros respectively. Scenario analyses to assess whether screening-specific disease high-risk populations would improve cost-effectiveness, showed that high-risk CVD populations were more likely to improve economic viability compared to COPD.
Screening for all Big-3 diseases simultaneously had the largest maximum acceptable cost (971 euros to 3,844 euros) per screened individual, depending on the WTP threshold. The maximum acceptable cost for Big-3 screening was substantially larger than screening for lung cancer only which was 113 euros to 341 euros, depending on the WTP. Results also showed that screening for lung cancer and CVD has a larger maximum acceptable cost than lung cancer and COPD screening (895 euros compared with 230 euros with a low WTP).
The higher maximum acceptable cost for screening for lung cancer and CVD compared to lung cancer and COPD, could be due to the limited benefits of early detection of COPD, where the most widely used treatment -- and only treatment in this model -- was smoking cessation, which is associated with poor adherence, delaying rather than preventing disease progression, the authors stated.
They highlighted that for breast and cervical cancer screening, costs have been estimated at 420 euros per screened individual, factoring in screening and diagnostic services, patient support, case management, program management, data management, and other smaller costs. This reference cost of breast and cervical cancer screening places Big-3 screening costs in a positive light, they reported.
The economic viability of combined screening is substantially larger than for lung cancer screening alone, due to benefits from CVD screening, noted the authors, but determining the target screening population is key to optimizing the program.
Future steps
The authors pointed to certain study limitations in terms of its optimistic analysis which assumed 100% sensitivity, specificity, and participation rate, assumptions which aligned to the goal of making an early-stage headroom analysis of potential cost-effectiveness to filter out non-cost-effective interventions. What was now needed was full cost-effectiveness analysis using real-world trial data, they stated.
For example, the maximum acceptable cost of Big-3 screening could be enlarged in a target screening population with high disease incidences and subsequently higher average health benefits per screened individual. In this study, the screening population had a high risk for one disease and a relatively high disease risk for all of the Big-3.
Further research is required to investigate cost-effectiveness based on prospective studies to explore an ideal target screening population and ideal recurrence of screening, Behr and colleagues concluded.