PET/CT images are offering evidence of a link between vascular patterns at the time of diagnosis for giant cell arteritis (GCA) and a patient's risk of an ischemic event, Spanish researchers explained in a study published online on 12 May in the European Journal of Nuclear Medicine and Molecular Imaging.
The group found that patients with inflammation in vertebral arteries, which causes blood vessels to narrow, were five times more likely to develop ischemic symptoms. The information may be particularly helpful because GCA is difficult to diagnose in its early stages.
"Bearing in mind these results and our findings, we consider that the vertebral arteries should be carefully studied in patients with suspected GCA, not only to support the diagnosis but also to assess the risk of development of ischemic events," wrote lead author Dr. Jaume Mestre-Torres and colleagues from Hospital Vall d'Hebron in Barcelona.
GCA's challenges
Giant cell arteritis is an inflammatory disease that causes the large blood vessels to narrow and restrict blood flow. The affliction is typically seen in the temporal arteries and the aorta in adults older than 50. Currently, there is little information on how the disease develops, although there are indications that it may be linked to genetics.
The challenge for clinicians is that there are "no specific clinical symptoms that lead to the diagnosis of GCA, but headache and ischemic symptoms such as jaw claudication and transient visual loss or permanent visual loss may raise suspicion [of the disease]," the authors noted.
Scanning temporal arteries with Doppler ultrasound has been shown to have good positive predictive value in patients with suspected GCA, and FDG-PET/CT can achieve good diagnostic accuracy for this clinical application, with previous research citing sensitivity of 83% and specificity of 89%. However, few studies are available that assess FDG-PET/CT's efficacy in detecting clinical signs and symptoms of the disease early in its development.
"The study of this field is critical, since it may have therapeutic and prognostic implications in daily clinical practice," Mestre-Torres and colleagues wrote. "The objective of the present study was to evaluate the existence of different patterns of vascular involvement on PET/CT in patients with GCA according to the presence or absence of ischemic manifestations at disease onset."
The investigators evaluated 21 women and nine men with a median age at diagnosis of 80.8 years (range, 72.7-84.4 years), who were diagnosed with GCA between January 2013 and January 2017. In all, 21 patients (70%) had ischemic manifestations and 13 (43%) had permanent visual loss (Eur J Nucl Med Mol Imaging, May 12. 2019).
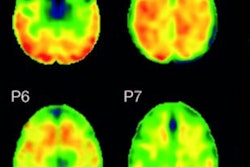
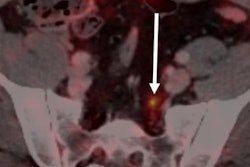
Images were acquired during the first 10 days of steroid therapy on a 64-slice CT and dedicated PET scanner (Biograph mCT, Siemens Healthineers) from the skull to both upper femurs following intravenous injection of 3.7 MBq/kg (222-370 MBq) of FDG. The results were interpreted by two nuclear medicine specialists who were blinded to all clinical information related to evidence of ocular and/or ischemic symptoms. Their analyses included the ascending aorta, aortic arch, descending aorta, abdominal aorta, carotid arteries, brachiocephalic trunk, vertebral arteries, subclavian arteries, and axillary arteries.
Through the PET/CT results, the researchers discovered that 23 patients (77%) had at least one vascular region with ischemia. The same number of patients exhibited large-vessel vasculitis, which included aortic and vertebral artery involvement. In addition, 18 patients (60%) were shown to have isolated involvement of the vertebral arteries. The remaining vascular territories -- the carotid arteries, subclavian arteries, brachiocephalic trunk, axillary arteries, and aorta -- were less frequently involved.
In assessing visual loss, the team found no significant differences between patients with vertebral artery involvement and permanent visual loss (61.5%) and patients with vertebral artery issues and no permanent visual loss (58.8%) (p = 0.88). Interestingly, the presence of intrathoracic large-vessel vasculitis tended to protect against a patient's likelihood of permanent visual loss.
In addition, "all patients with vertebral involvement but no aortic involvement showed ischemic manifestations at disease onset," the researchers noted. "In contrast, none of the patients with aortic involvement but no vertebral hypermetabolism showed ischemic symptoms."
Based on the level of arterial inflammation among all regions assessed by PET/CT, they determined that an ischemic event was most likely to occur among patients with vertebral artery involvement, with a calculated odds ratio of 5.0 (p = 0.05).
"We believe that our findings may have therapeutic and prognostic implications in daily clinical practice," Mestre-Torres and colleagues concluded. "Future research is needed to establish the role of PET/CT in diagnosing GCA and assessing the risk of ischemic events at disease onset. Finally, the inclusion of this technique in the GCA classification criteria should be considered."