Performing breast MRI on patients in the supine position more accurately determines breast cancer tumor size than prone MRI, according to research from Finland. And because supine MRI demarcates and projects lesions on the skin in the same position used in surgery, it is likely to reduce the need for more operations.
The study compared supine and prone breast MRI in breast cancer patients scheduled for oncoplastic breast-conserving surgery. Supine MRI was less likely to overestimate tumor size than prone MRI, according to a research team led by Dr. Sarianna Joukainen from the surgery department and Dr. Amro Masarwah, PhD, from the clinical radiology department at Kuopio University Hospital.
"Supine MRI more accurately determines the size of the tumors compared with prone MRI and might have an important role in diminishing overestimations," the authors wrote (European Radiology, 17 August 2018) "Supine MRI enables the lesions detected in prone MRI to be demarcated and projected on the skin in the same position used in surgery. This practically ensures the proper estimation of the resection area."
Doing so means MRI might reduce the number of reoperations due to possible positive margins, they added.
Supine vs. prone breast MRI
Preoperative MRI for patients scheduled for breast-conserving surgery can reveal additional information about the size, shape, location, and possible multifocality or multicentricity of the breast tumor.
"The traditional diagnostic methods, i.e., mammography and ultrasound, are usually insufficient to show the true extent of the disease, while MRI is the best diagnostic method," Joukainen told AuntMinnieEurope.com.
MRI can help guide the extent of surgical excision, therefore reducing reoperation rates for positive margins. MRI is routinely performed in the prone position, while surgery is performed with the patient lying in the supine position, resulting in displaced or deformed breast tumors.
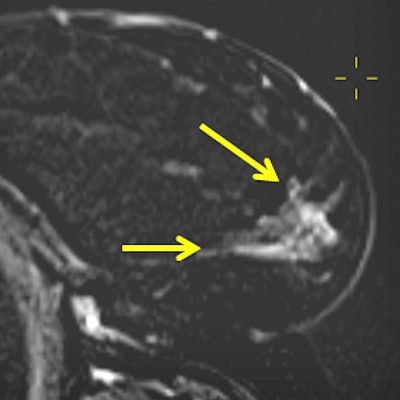
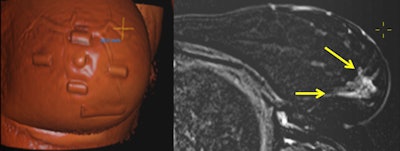 A 41-year-old patient with a large multifocal ductal cancer in the lower lateral quadrant of the left breast. Preoperative prone MRI showed a new large area of segmental nonmass enhancement in the upper quadrant of the same breast (not shown). A shaded, volume-rendered reconstruction image of supine MRI side by side to an axial subtraction image allows physicians to visualize the MRI-only detected lesions (arrows) in the surgical position and also navigate in real-time through the lesion and appreciate its extent as projected by a "crosshair" tool on the skin, also allowing measurements of distances in relation to the MRI-visible capsules positioned on the skin before scanning. All images courtesy of Dr. Sarianna Joukainen.
A 41-year-old patient with a large multifocal ductal cancer in the lower lateral quadrant of the left breast. Preoperative prone MRI showed a new large area of segmental nonmass enhancement in the upper quadrant of the same breast (not shown). A shaded, volume-rendered reconstruction image of supine MRI side by side to an axial subtraction image allows physicians to visualize the MRI-only detected lesions (arrows) in the surgical position and also navigate in real-time through the lesion and appreciate its extent as projected by a "crosshair" tool on the skin, also allowing measurements of distances in relation to the MRI-visible capsules positioned on the skin before scanning. All images courtesy of Dr. Sarianna Joukainen."In our opinion, the failure to show the true benefits of breast MRI is not only related to the microscopic tumor burden, but also to our inability to translate the information obtained from imaging in the prone position to surgery in the supine position," the study authors wrote.
Clinicians shy away from supine MRI because breast consistency, shape, and size differ among patients, and thus the supine breast position cannot be individually predicted on the basis of prone MRI studies alone. MRI radiofrequency coils must be flexible to adjust for each individual breast. Also, chest wall movement during breathing requires an ultrafast sequence.
So far, few reports exist that deal with the positioning dilemma and transference of this information to the operating theater. So Joukainen, Masarwah, and colleagues sought to prospectively evaluate the feasibility of preoperative supine MRI using commercially available coils and breath-hold sequences to create accurate tools to transfer this information to breast surgeons using drawing charts and skin ink mark projections.
The researchers included 14 consecutive patients from Kuopio University Hospital, analyzing 15 breasts and 27 lesions (19 mass and eight nonmass). In addition to a diagnostic prone breast MRI scan (Philips Achieva 3.0T TX, Philips Healthcare), a supplementary supine 1.5-tesla MRI exam (Siemens Magnetom Aera, Siemens Healthineers) was performed with the patient in the surgical position, including skin markers.
Tumor locations were ink-marked on the skin according to findings obtained from supine MRI. The researchers measured changes in the tumors' largest diameter and locations between prone and supine MRI and compared them with histology. They also measured nipple-to-tumor and tumor-to-chest wall distances. Tumors and suspicious areas were surgically removed according to skin ink markings.
| Prone vs. supine breast MRI in breast-conserving surgery patients* |
||
| Prone MRI | Supine MRI | |
| Overestimation of tumor size | 47.1% | 14.5% |
| Difference in mean diameters and areas | -38.3% | -20.9% |
| Nonmass lesion difference | -9.2% | -31.2% |
In addition, the tumors' mean distance from the chest wall diminished by 69.4% and from the nipple by 18.2% using supine MRI.
The results consistently show significantly smaller lesion sizes when measured from supine MRI as compared with prone MRI, the authors stated. A possible reason is an "accordion-like" mechanism: In the prone position, closely located ductal structures broaden out and track surrounding tissues, resulting in discontinuous and fragmented areas of enhancement, they explained.
Solid breast tumors are much stiffer than the normal breast parenchyma, and the "accordion effect" occurs mainly in the peritumoral area, meaning size changes are minimal in solid lesions (mean 9.2%) as compared with nonmass lesions (20.9%), they added.
"Results were quite what we anticipated, but the magnitude of changes surprised us a little," Joukainen told AuntMinnieEurope.com. "It was fascinating to notice how supine MRI pinpointed the location of even the smallest visible, multifocal tumors. We have noticed patients feel more comfortable knowing that we are trying to remove every possible visible tumor."
Joukainen and colleagues will "definitely" incorporate the protocol in their routine clinical practice after completing the new surgical continuation study using supine MRI-guided surgery.
"We now are more confident in achieving negative margins in these complex situations," she stated. "Hopefully many will find this application useful."