The European Society of Breast Imaging (EUSOBI) has released a new set of guidelines for breast ultrasound. Among the key recommendations is that ultrasound alone is not sufficient for breast screening, despite the limitations of mammography
The EUSOBI board conducted an extensive literature review of breast ultrasound and then ran the document past patient groups to draft the paper published online on 9 August by Insights into Imaging. This is the third in a series from EUSOBI.
 Dr. Andy Evans from the University of Dundee.
Dr. Andy Evans from the University of Dundee."This series is about empowering patients by helping them understand what the strengths and limitations of breast imaging modalities are," leader author Dr. Andy Evans, a breast imaging professor at the University of Dundee in U.K., told AuntMinnieEurope.com.
"This should help patients be more confident that they have been referred for the right test and enable them to question when they have been referred for an inappropriate test," he added. "Life would be easy if diagnostic tests were 100% accurate; obviously this is not the case, but educating patients as to the confidence they should have in their imaging test result is also important."
The ins and outs of ultrasound
EUSOBI's report is addressed primarily to women themselves and physicians dealing with patients for whom breast ultrasound is being, or may be, considered. Seven special information notes and five frequently asked questions are formatted for use in direct communication with women.
"Considering the relevant differences across European countries in terms of available technology, national guidelines, clinical practices, healthcare systems, and insurance coverage, these recommendations can have different applications under local conditions," Evans and colleagues wrote.
They searched for information on breast ultrasound published from January 2007 to December 2017. After deciding which articles to base their recommendations on, the entire text underwent a double evaluation by the authors, each of whom contributed with relevant content.
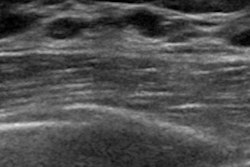
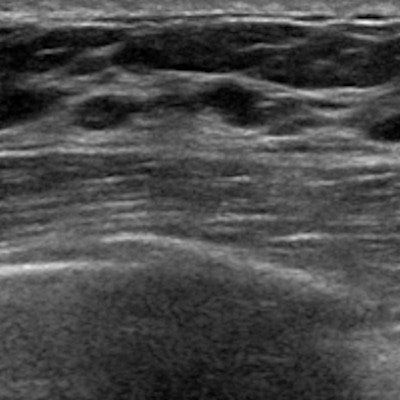
The report covers safety, quality, the examination itself, and the various techniques, including automated breast ultrasound.
"If the woman is examined with this technique, it's important to remember that the report is the result of an evaluation performed by a radiologist in a separate session, and that, if a suspicious finding is detected, the woman has to be recalled and a work-up with targeted handheld ultrasound is necessary," the authors noted.
Optimum use
Evans and colleagues also define when to use breast ultrasound. In high-risk women who cannot undergo screening with MRI, ultrasound is indicated for women younger than 35 years old and as an adjunct to mammography in older women.
For BRCA mutation carriers, evidence of higher sensitivity to radiation exposure of the breast tissue suggests avoiding mammography, at least at a younger age. In women who have an average or intermediate risk with dense breasts, supplemental screening with either handheld or automated bilateral breast ultrasound can be performed after a negative mammogram to increase cancer detection, the authors noted.
Some studies demonstrate ultrasound can detect breast cancers in asymptomatic women with heterogeneously or extremely dense breasts, but that doesn't mean it can replace mammography just yet.
"Adjunctive ultrasound screening can detect biologically important cancers, but there is not sufficient evidence in favor of adopting adjunctive ultrasound screening as a general policy," they wrote. "Well-designed large studies with sufficient follow-up are needed."
The report also covers the following indications for breast ultrasound:
- Palpable lump
- Axillary adenopathy
- First diagnostic approach for clinical abnormalities for women younger than age 40 and in pregnant or lactating women
- Suspicious abnormalities at mammography or MRI
- Suspicious nipple discharge
- Recent nipple inversion
- Skin retraction
- Breast inflammation
- Abnormalities in the area of the surgical scar after breast-conserving surgery or mastectomy abnormalities in the presence of breast implants
- Screening high-risk women, especially when MRI is not performed
- And more
In addition, the authors also answered the following five frequently asked questions:
- Is breast ultrasound a harmless investigation?
- Can breast ultrasound be performed instead of mammography for breast cancer screening in the general female population, as it spares radiation?
- After a breast ultrasound examination, does the woman also need mammography?
- Can women consider breast ultrasound being free from any potential negative consequences?
- After receiving the result of a breast handheld ultrasound, can women try to get a reliable second opinion on the test?
Talk to radiologists, the authors advise.
"Do not hesitate to discuss unclear issues of your ultrasound examination with your breast radiologist," they noted. "Do this in particular in the case of U3 or BI-RADS 3, if you are wondering about the need to undergo a needle biopsy, or you are thinking of postponing the needle biopsy, as well as in the case of U4/BI-RADS 4 or U5/BI-RADS 5 and when further imaging workup is suggested (e.g., digital breast tomosynthesis, MRI)."
Breast ultrasound is safe and widely available for breast imaging, and this document should clear up any confusion, they concluded.