The use of the radiopharmaceutical fluorine-18 dihydroxyphenylalanine (F-18 DOPA) with PET imaging can lead to beneficial changes in management plans for patients with brain tumors, according to a study presented by French researchers at the recent Society of Nuclear Medicine and Molecular Imaging (SNMMI) meeting.
The prospective study of more than 100 patients found that F-18 DOPA-PET changed treatment decisions in 34% of cases, leading to either an increase in treatment from the initial diagnosis of radiation necrosis to tumor recurrence or a decrease in treatment based on a downgrade to radiation necrosis.
"F-18 DOPA-PET imaging is a patient- and physician-friendly exam. For the patient, it is a 20-minute postinjection acquisition, and [the patient] stays under the camera for only 10 minutes," said study co-author Dr. Olivier Humbert, PhD, from the Centre Antoine Lacassagne in Nice. "For the physician, the visual analysis is easy and is done using total uptake as a reference."
F-18 DOPA applications
Previous literature has shown that F-18 DOPA-PET is useful in making initial diagnoses of primary brain tumors. It also has been suggested that the imaging technique could enhance accuracy in the diagnosis of tumor recurrence after treatment and to differentiate radiation necrosis from tumor relapse. In fact, F-18 DOPA has approval in France for investigating such cancer recurrence.
 Dr. Olivier Humbert, PhD, from the Centre Antoine Lacassagne in Nice, France.
Dr. Olivier Humbert, PhD, from the Centre Antoine Lacassagne in Nice, France.Furthermore, F-18 DOPA-PET has become a better diagnostic tool than MRI in these cases, since differentiating between recurrence and radiation necrosis is often difficult on MRI during the follow-up of patients treated for malignant brain tumors.
"The aims of this prospective study were to assess the clinical impact of F-18 DOPA-PET in the management of brain tumor patients with suspicion of recurrence," Humbert told SNMMI meeting attendees. "We also tried to compare the PET and pathological findings, if surgery was finally performed."
In this prospective study, researchers evaluated 111 patients with a mean age of 58 years with a total of 143 cases. In some cases, patients were evaluated more than once for different suspicions of recurrence. Among the subjects were 55 glioblastomas, 10 grade III and 11 grade II primary brain tumors, and 35 metastases.
All patients had been treated previously for a brain tumor and were included in this study because of a suspicion of recurrence during the follow-up. The subjects underwent two brain imaging scans performed within no more than four weeks. They were evaluated by F-18 DOPA-PET after initial treatment with surgery, radiation therapy, and/or chemotherapy to determine if changes in treatment management were warranted.
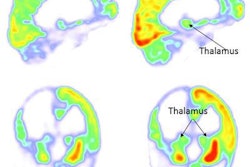
A 10-minute static PET/CT scan (mCT, Siemens Healthineers) was performed 20 minutes after injection of 2 MBq/kg of F-18 DOPA. T1-weighted MR images were coregistered to PET data.
Images are graded visually on a scale from 0 to 3: 0 for a lesion not visible, 1 for uptake less than the striatum, 2 for lesion uptake equal to the striatum, and 3 for uptake greater than the striatum. PET images were deemed positive for a score greater than 1.
"With F-18 DOPA, one advantage is that the striatum's physiological uptake can be used as an internal reference to analyze lesion uptake so as to distinguish a DOPA-negative lesion from a DOPA-positive one," Humbert said.
Image results typically are evaluated during the weekly multidisciplinary neuro-oncology committee meetings on how to proceed with patient treatment. Final decisions are based on MRI data, which includes perfusion and spectrometry, and F-18 DOPA-PET images, which are coregistered to MR images.
"According to the aims of this study, we first analyzed the number of changes in treatment induced by F-18 DOPA-PET," he added. "If there was no change of treatment, then the level of confidence of the decision to treat [the patient] was recorded. If surgery was performed, we compared the PET and pathological findings."
Key numbers
Most important, F-18 DPOA-PET changed treatment decisions in a major way for 48 (34%) of the 134 cases. In 38 cases (80%), there was an increase in treatment as the initial diagnosis was upgraded from a radiation necrosis to tumor recurrence based on positive F-18 DOPA-PET results. For the other 10 patients (20%), their diagnoses of tumor recurrence were downgraded to radiation necrosis.
For the remaining 65 patients (68%), F-18 DOPA-PET did not change treatment. Among the patients whose management was unchanged, the confidence level of the initial treatment decisions increased in 23 cases (16%), compared with the level of confidence decreasing for seven cases (5%).
Among 26 patients who later underwent surgery, recurrence was the reason for 21 patients (80%), with F-18 DOPA-PET results as positive. Among the other five patients (20%) who underwent surgery for radiation necrosis, three patients (60%) had negative F-18 DOPA-PET results and two (40%) were positive.
"That means these patients should not have been operated on," Humbert said. "MRI was falsely positive in these five cases. In contrast, PET was falsely positive only in two of these patients."
Based on the results, the authors concluded that F-18-DOPA-PET appeals to both patients and physicians due to its short image acquisition time and the ease of visual analysis of total uptake to make treatment decisions.