A growing number of reports eloquently speak about explorations into 7-tesla MRI, with the goal of making the transition to the clinic. This progress is no great surprise, but a number of challenges remain. These unsolved problems should not be hidden under the carpet, but rather act as a surface marker thanks to contributions made by forward-thinking scientists, clinicians, and healthcare program managers.
This faith attracts resources and invites talent, all putting further weight behind solving the conundrum governed by the physics and engineering, with the ultimate goal to harmonize development of novel imaging technology and costs with added clinical value, simplicity, and ease of use. Meanwhile, the pace of discovery is heartening and a powerful motivator to transfer the lessons learned at 7 tesla from basic research into the clinical scenario. These efforts are fueled by the unmet clinical needs and the quest for advancing the capabilities of diagnostic MRI -- today.
The novel technology tailored for 7-tesla MRI, together with the eye-opening quality of the anatomical and functional images, created excitement among the imaging community and is the driving force for broader clinical studies. Already, recognition of the benefits and performance of ultrahigh-field MR technology is resulting in a migration to 3 tesla, where many of the issues surfacing at 7 tesla, though somewhat reduced, remain significant.
This migration is a game changer versus the somewhat suboptimal copy/paste approach previously used to move MRI techniques/protocols from 1.5 to 3.0 tesla, and hence continues to inspire clinical research. The migration alone has earned 7 tesla the moniker of being a steam engine for innovation.
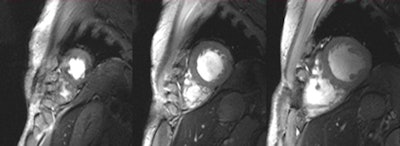
![Set of six (top and bottom) 2D CINE FLASH images of the beating human heart derived at systole from a series of 12 short-axis views ranging from the apex to the base of the heart (in-plane resolution [1 x 1] mm2, slice thickness of 4 mm, acceleration factor = 2, GRAPPA). A 2D 16-channel transmit/receive radiofrequency coil array was used for signal transmission and reception.6 The images illustrate that a rather uniform intensity distribution was obtained across the entire heart.6](https://img.auntminnieeurope.com/files/base/smg/all/image/2012/06/ame.2012_05_31_11_45_47_702_2012_06_01_niendorf_image1b.png?auto=format%2Ccompress&fit=max&q=70&w=400) Set of six (top and bottom) 2D CINE FLASH images of the beating human heart derived at systole from a series of 12 short-axis views ranging from the apex to the base of the heart (in-plane resolution [1 x 1] mm2, slice thickness of 4 mm, acceleration factor = 2, GRAPPA). A 2D 16-channel transmit/receive radiofrequency coil array was used for signal transmission and reception.6 The images illustrate that a rather uniform intensity distribution was obtained across the entire heart.6
Set of six (top and bottom) 2D CINE FLASH images of the beating human heart derived at systole from a series of 12 short-axis views ranging from the apex to the base of the heart (in-plane resolution [1 x 1] mm2, slice thickness of 4 mm, acceleration factor = 2, GRAPPA). A 2D 16-channel transmit/receive radiofrequency coil array was used for signal transmission and reception.6 The images illustrate that a rather uniform intensity distribution was obtained across the entire heart.6Admittedly, the reports put forward by numerous pioneers and early clinical adopters are so far largely anecdotal. It is a fractal pattern, though, and a consistent story is starting to emerge -- a story worth following since its clinical implications feed into a broad spectrum of neurology, neuroscience, neuroradiology, radiology, cardiology, and other fields of clinical research. This story includes a chapter that comprises around 150 abstracts presented at the recent 20th annual meeting of the International Society of MR in Medicine (ISMRM) held in Melbourne, Australia, and more than 100 clinical research papers published since 2010.
An exciting development in clinical research is that cutting-edge MR centers are pushing the boundaries by investigating the feasibility and clinical value of 7-tesla MRI for imaging neurodegenerative and neuroinflammatory diseases. Here, increasing the field strength helps to gain signal-to-noise ratio, contrast-to-noise ratio, and spatial resolution, which are all currencies of diagnostic image quality.
In particular, enhanced spatial resolution can help to advance the capabilities of imaging subtle focal cerebral lesions. A recent study demonstrated in a side-by-side analysis that MPRAGE MRI at 7 tesla depicted 82% more subtle multiple sclerosis (MS) lesions than MPRAGE MRI at 1.5 tesla due to the enhanced T1 contrast and the high spatial resolution.1
These improvements can be also put to clinical use to detect lesions at an earlier stage of disease progression, if not prior to the onset of clinical symptoms. This capability has been demonstrated by MR microscopy of animal models, using an effective resolution (pixel per anatomy) currently approached in humans with 7-tesla MRI.2 Also, it offers means for differential diagnosis.
Cerebral lesions morphology derived from 7-tesla exams differentiates Susac syndrome (an orphan disease that needs to be considered in the differential diagnostic workup of various neurological disorders) from MS, according to a recent clinical study. This study demonstrated that white matter and callosal lesion morphology in Susac syndrome differs significantly from MS plaques in terms of a perivascular localization, the presence of a hypointense ring, and the frequency of CSF-isointense lesions, as illustrated in figure 2.3
Also, the (super)linear relationship between magnetic field strength and sensitivity for susceptibility effects in T2*-weighted imaging, together with the enhanced spatial resolution, can substantially enhance the detection of anatomical details of MS plaques.
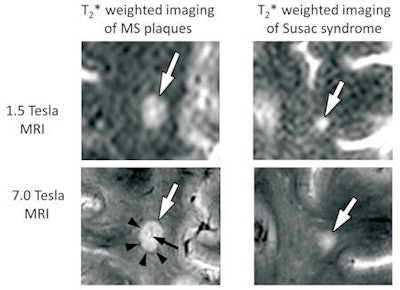 Examples of T2*-weighted imaging of multiple sclerosis (MS) (left) versus Susac syndrome (right) white-matter lesions at 1.5 tesla (top) and 7 tesla (bottom). At 1.5 tesla, both MS and Susac syndrome white-matter lesions (white arrow) appear similar as hyperintense lesions.3 Due to the enhanced signal-to-noise ratio, contrast-to-noise ratio, and improved spatial resolution at 7 tesla, ultrahigh-field MRI reveals distinctive lesion morphology: MS lesions are characterized by a central vein (black arrow) and in particular a hypointense rim (arrow head). In comparison, white-matter lesions in Susac syndrome do not show a hypointense rim, and therefore appear blurry. Perivenous arrangement is not a typical feature of Susac syndrome lesions but can coincidentally occur with veins being most likely located peripherally.3
Examples of T2*-weighted imaging of multiple sclerosis (MS) (left) versus Susac syndrome (right) white-matter lesions at 1.5 tesla (top) and 7 tesla (bottom). At 1.5 tesla, both MS and Susac syndrome white-matter lesions (white arrow) appear similar as hyperintense lesions.3 Due to the enhanced signal-to-noise ratio, contrast-to-noise ratio, and improved spatial resolution at 7 tesla, ultrahigh-field MRI reveals distinctive lesion morphology: MS lesions are characterized by a central vein (black arrow) and in particular a hypointense rim (arrow head). In comparison, white-matter lesions in Susac syndrome do not show a hypointense rim, and therefore appear blurry. Perivenous arrangement is not a typical feature of Susac syndrome lesions but can coincidentally occur with veins being most likely located peripherally.3Another report has demonstrated distinct lesion morphology at 7-tesla MRI that supports differentiation of neuromyelits optica spectrum disorders (NMOSD) from MS. The authors observed differences between cortical gray- and white-matter lesions of NMOSD versus MS, findings that the technique may serve as an imaging marker to distinguish NMOSD from MS and underscore the distinct underlying disease pathology.4 Bearing these reports in mind, 7-tesla MRI promises to provide insights into the pathophysiology and pathogenesis of lesions.
At the same time, this research is paralleled by pioneering explorations into human stroke imaging and imaging microbleeds at 7 tesla. Stroke lesions visible at 3 tesla can all be detected at 7 tesla.5 Improved spatial resolution at 7 tesla helps to reveal more anatomical detail and pathophysiological characteristics of ischemic lesions, which pays off for imaging microinfarcts. These findings encourage further exploration into the diagnostic benefits that 7-tesla MRI may offer for neurology and neuroradiology.
It is no secret that the feasibility of 7-tesla MRI is not limited to the brain, but also can be beneficial for musculoskeletal and cardiac imaging. The requirements of cardiac MR at 7 tesla inspired recent advances in multichannel radiofrequency (RF) coil technology. This includes the move from cardiac optimized RF coils equipped with four transmit/receive channels only to 16 TX/RX channels configurations,6 and even 32 TX/RX channel versions.7
It has been shown that a larger number of elements, in conjunction with a 2D RF coil-array design, can improve image quality, as well as accelerated imaging performance.8 All these efforts culminated in images of the beating heart with a spatial resolution that is by an order of magnitude superior to that routinely available at 1.5 tesla.
These improvements offer detailed insights into cardiac anatomy and might provide means for a better understanding of the myocardial microstructure. Recognition of the benefits of the many channel RF coil configurations should help to eventually lead to a 7-tesla body RF coil design, though this is, for the moment, merely a vision. It is nonetheless a vision that offers the potential to inspire a further push toward body imaging at 7 tesla.
In short, today's ultrahigh-field MR developments and clinical applications are intriguing and in a creative state of flux. Hoofing ultrahigh-field MR into the clinic remains challenging, but the race has started already, with the early adopters approaching the finish line in a speedy gallop.
For more information on this area, you may want to attend the 3rd Annual Scientific Symposium on Ultrahigh Field (UHF) Magnetic Resonance: Clinical Needs, Research Promises, and Technical Solutions, which will be held on 8 June 2012 at the Max-Delbrueck-Center for Molecular Medicine in Berlin. The meeting has had official endorsement from the ISMRM and the European Society for MR in Medicine and Biology. For free registration, please go to www.uhf-mr.de.
Dr. Thoralf Niendorf is a professor for experimental ultrahigh-field magnetic resonance at Charité - University Medicine Berlin and the director of the Berlin Ultrahigh Field Facility (B.U.F.F.) at the Max-Delbrueck-Center for Molecular Medicine.
References
- Sinnecker T, Mittelstaedt P, Dörr J, et al. Multiple sclerosis lesions and irreversible brain tissue damage: A comparative ultrahigh-field strength magnetic resonance imaging study [published online ahead of print 20 February 2012]. Arch Neurol. 2012. http://archneur.jamanetwork.com/article.aspx?doi=10.1001/archneurol.2011.2450.
- Waiczies H, Millward JM, Lepore S, et al. Identification of cellular infiltrates during early stages of brain inflammation with magnetic resonance microscopy. PLoS One. 2012;7(3):e32796.
- Sinnecker T, Wuerfel J, Niendorf T, Paul F, Kleffner I, Dörr J. Lesion Morphology at 7-tesla MRI Differentiates Susac Syndrome from Multiple Sclerosis. Proceedings of the ISMRM 2012 #821.
- Sinnecker T, Dörr J, Pfueller CF, et al. Distinct lesion morphology at 7T MRI differentiates neuromyelitis optica from multiple sclerosis. Neurology. 2012 in press.
- Madai VI, von Samson-Himmelstjerna FC, Bauer M, et al. Ultrahigh-field MRI in human ischemic stroke -- a 7 tesla study. PLoS One. 2012;7(5):e37631.
- Thalhammer C, Renz W, Pfeiffer H, et al. A two-dimensional sixteen channel transmit/receive coil array for cardiac MRI at 7.0 tesla: Design, evaluation and application. J Magn Reson Imaging. 2012 in press.
- Gräßl A, Renz W, Hezel F, et al. Design, Evaluation and Application of a Modular 32 Channel Transmit/Receive Surface Coil Array for Cardiac MRI at 7-tesla. Proceedings of the ISMRM 2012 #305.
- Winter L, Kellman P, Renz W, et al. Comparison of three multichannel transmit/receive radiofrequency coil configurations for anatomic and functional cardiac MRI at 7.0-tesla: Implications for clinical imaging. Eur Radiol. 2012 in press.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.