The use of respiratory-gating techniques during free breathing while delivering radiation therapy for tumors close to the diaphragm reduces the exposure of healthy tissue to radiation. However, treatment delivery times are longer -- increasing patient risk and potentially causing scheduling problems for radiation therapy departments.
Researchers at the Universitair Ziekenhuis Brussel in Brussels may have found a solution in an inexpensive, low-tech technique that has improved their use of respiratory gating. Having patients use visually guided voluntary breath-hold along with audio assistance has slashed treatment time duration at the Belgian oncology center, so that it's comparable to conventional treatment times. The results of their efforts are detailed in an article in press in Radiotherapy & Oncology (April 15, 2009).
Respiratory gating during free breathing is a technique to reduce the body's internal motion while receiving radiation therapy for tumors near the diaphragm that are subject to respiratory motion from breathing. When irradiation is limited to a part of the breathing cycle, the motion of the tumor is also limited. This enables radiation dose delivery to be more precise and margins surrounding the tumor to be reduced, thus sparing more normal tissue.
The disadvantage of this technique is that treatment using free breathing takes longer than breath-hold techniques. Radiation oncology departments operating at near capacity may find it difficult to schedule and accommodate these patients, as was the case at the Universitair Ziekenhuis Brussel Oncology Center.
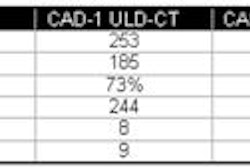
In 2005, the radiation oncology team decided to see if adding visual feedback with audio prompting or visual feedback alone could decrease treatment time compared to patients not receiving feedback. Between August 2005 and April 2008, 25 patients had respiratory-gated radiation therapy. Nine patients were irradiated during free breathing with no feedback, seven received visual feedback only, and nine received visual feedback with audio assistance.
Treatment time duration for the group receiving visual feedback with audio assistance decreased by 47% compared to patients receiving no feedback. With visual feedback only, treatment time duration showed a more modest improvement of 17.6% over the no-feedback group.
Because the composition of each group differed, and treatments were different, the researchers normalized the treatment times to the amount of minutes required to deliver 100 MU, according to lead author and medical physicist Nadine Linthout, Ph.D. This normalization also compensated for the differences in tumor depth, tumor size, and other tumor-related characteristics.
Tumor types and treatment by group and number of patients
|
Treatment planning was performed with BrainScan v5.3 (BrainLab, Munich, Germany) on a CT dataset acquired during free breathing, with a slice thickness of 2.5 mm and a slice spacing of 2.5 mm covering the entire thoracic region. All patients were treated with conformal-beam therapy, with an average of seven (range, five to 10) coplanar nonmodulated static conformal beams delivered at a dose rate of 480 MU/min.
Constraints for the planning target volume were identical for all patients, with 95% of the volume receiving 95% of the prescribed dose, 99% of the volume receiving 90% of the prescribed dose, and a maximum of 15% of the volume receiving 105% of the prescribed dose.
During treatment, infrared markers were placed on either the patient's thorax or abdomen, depending upon which showed the most movement during breathing. The system (ExacTrac5.0/Novalis Body, BrainLab) that calculated patient positioning and determined target location detected the movement of the markers and obtained a usable breathing signal from the movement. The gating was performed at the exhale phase of breathing.
Patients were trained in advance on use of the visual and audio aids. Eye-Trek FMD-200 video glasses (Olympus, Tokyo) enabled patients to follow their own breathing signals and displayed a beam-on-area signal in the breathing cycle. Patients were asked to perform a breath-hold in the beam-on-area or to limit their breathing amplitude at this time.
When earphones were added, audio coaching was used to help the patient perform a breath-hold in the beam-on-area signal. Patients also were told when to perform free breathing during target localization verification and linac setup.
The delivery time for a gated treatment during free breathing was 1.7 min/100 MU on average. This was reduced to 1.4 min/100 MU with visual feedback and to 0.9 min/100 MU with visual feedback and audio assistance. The treatment times achieved with visual feedback alone approximated the delivery time of conventional coplanar intensity-modulated radiation therapy not hampered by the breathing of the patient.
After this study was completed, the radiation therapy department decided to increase the default dose rate from 480 MU/min to 800 MU/min. Patients are now receiving this higher dose using the visual feedback with audio coaching. The average treatment time has been decreased to 0.4 min/100 MU.
By Cynthia E. Keen
AuntMinnie.com staff writer
May 19, 2009
Related Reading
Infrared sensors track radiation treatment in India, September 11, 2008
Copyright © 2009 AuntMinnie.com