Brain metastases are a frequent occurrence in lung cancer patients, and a CT scan is often ordered to find them. But if a whole-body PET/CT scan is already available from the original workup, there's no need for the extra expense and radiation of a dedicated CT scan, according to researchers from Belgium, who found that the CT portion of the PET/CT scan is enough for the initial diagnosis.
For staging lung cancer tumors, lymph nodes, and metastases, CT is the preferred modality in many hospitals because of the high-quality, fast anatomic information it provides. PET, when available, can also be used to evaluate lymph nodes and metastases. And with the addition of CT in hybrid scanners, it's becoming a universal test, said Dr. Walter De Wever from University Hospitals Leuven in Belgium.
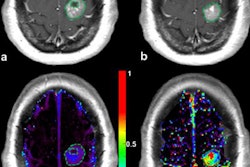
PET/CT has already proved its worth as the best imaging technique for evaluating tumors in the liver, adrenal glands, and bones, but questions remain about its utility in the brain, De Wever said at the 2009 European Congress of Radiology (ECR) in Vienna. The researchers decided to examine the modality's value for the evaluation of brain metastasis compared to dedicated CT.
De Wever and his team examined scans from 123 lung cancer patients between 2004 and 2006, 87 of whom had both integrated PET/CT and a dedicated CT of the head to look for metastases. Both CT studies used contrast enhancement. PET/CT was performed on a dual-modality PET/CT scanner (Biograph Duo LSO, Siemens Healthcare, Erlangen, Germany) with a two-detector-row CT component (85 mAs, 130 kV, 5-mm slice thickness). Whole-body PET images were acquired 75 minutes after FDG injection.
The dedicated CT images were acquired at 380 mAs, 120 kV, and a collimation of 24 x 1.2 mm (slice thickness, 2.4 mm).
Of the 87 patients (54 men, 33 women; mean age, 58 years) included in the retrospective study, 49 (56%) had primary lung cancer and the remaining 27 (44%) patients were examined with CT due to neurological symptoms.
"The final diagnosis of the presence or absence of brain metastasis was based on the dedicated CT of the brain, and maybe also additional information from MRI and follow-up," De Wever explained.
Both the dedicated CT scans (CT1) and the CT component of PET/CT (CT2) were evaluated by two experienced neuroradiologists on the detection of brain lesions (benign and malignant), with an interval of at least two weeks between examinations of CT datasets. The readers were blinded to clinical information and to the images in the other CT scan.
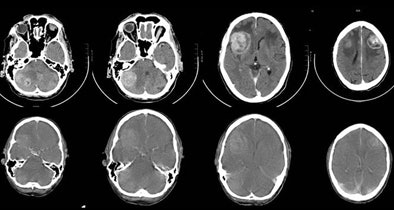 |
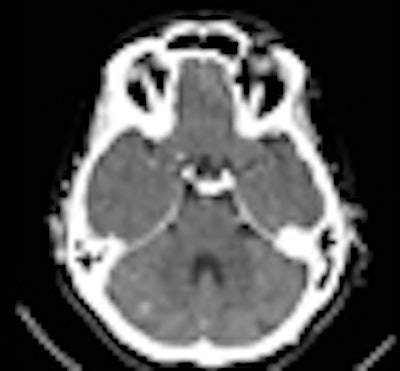
| A 67-year-old man with small cell lung cancer in the left upper lobe also developed neurological symptoms. Diagnostic brain CT (upper row) showed multiple brain metastases: two right cerebellar, one right frontal, and one left frontal, all surrounded by edema. The CT component of the integrated PET/CT (lower row) also showed brain metastases but could not demonstrate one right cerebellar metastasis (first image). The quality of the CT of the PET/CT is inferior to that of diagnostic brain CT. There is reduced contrast opacification and the surrounded edema is not clearly visualized, although this could have been due to the treatment with corticosteroids in the short time between diagnostic brain CT and integrated PET/CT. All images and charts courtesy of Dr. Walter De Wever. |
The PET/CT scans were also evaluated by a radiologist and a nuclear medicine specialist working in consensus. The results of PET/CT and the two CT scans were correlated, and both readings were compared with the final diagnosis. Statistical analysis was performed by measuring sensitivity, specificity, positive and negative predictive values, and accuracy.
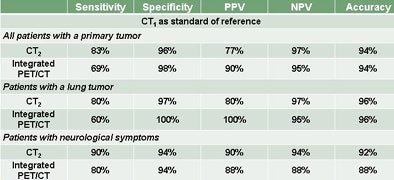
In all, there were 15 patients with malignant lesions, including 12 with brain metastases and three with bronchial tumors, De Wever said. Among the patients with lung tumors, only six had malignant lesions, all brain metastases. In this group, there were eight patients with symptoms suspicious for brain lesions, and four of these were found to have brain metastases.
"We had false negatives in both techniques," he said. "Only patients who had clinical symptoms [of neurological deficit] had all of the brain metastases detected."
In all patients, the dedicated CT showed 12 true positives and three false negatives, while the CT component of PET/CT showed 10 true positives and five false negatives.
The value of the CT component of PET/CT was superior to integrated PET/CT -- probably due to differences in the experience of the readers: neuroradiologists for the CT component of PET/CT versus general radiologists in consensus with a nuclear medicine physician for PET/CT, De Wever said.
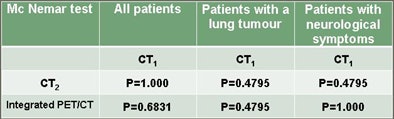
"When we use the final clinical diagnosis, we get the same results," he said. "The CT part of PET/CT was better than integrated PET/CT, but there was also a little bit of difference between the diagnostic CT and the CT part of PET/CT, probably due to [differences in] the quality of images." Still, no significant difference was found between CT1 and CT2.
"We can say that when we do [whole-body] PET/CT, we have a PET/CT of the brain without additional costs," he said. Comparing the dedicated CT scan with the CT portion of the PET/CT, "we could not find a statistically significant difference despite the fact that the quality of the brain PET/CT was inferior to the dedicated CT of the brain."
 |
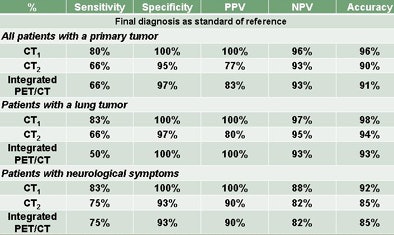 |
| Comparison of dedicated CT of the brain (CT1) versus the CT component of PET/CT (CT2) shows no statistically significant difference between these two CT scans in detecting malignant brain lesions, despite the fact that the quality of the CT of the brain in the PET/CT study is inferior. |
 |
The results suggest that there is no need to do a dedicated CT of the brain when PET/CT is available, especially in patients with symptoms suspicious for brain metastases. Brain MRI might be more appropriate for further evaluation in such cases, he said.
By Eric Barnes
AuntMinnie.com staff writer
April 2, 2009
Related Reading
Radiosensitizers generally do not make whole-brain radiotherapy more effective, January 28, 2009
Inversion-recovery MRI falls short in brain tumor detection, February 27, 2008
MRI, PET/CT show different strengths in tumor staging, January 26, 2006
PET/CT shows potential for detecting unknown primary cancers, December 8, 2005
Copyright © 2009 AuntMinnie.com