A key strength of MRI is it allows accurate anatomic and functional evaluation of the three pelvic compartments, enabling the correct identification of the compartments involved, according to award-winning Portuguese researchers. It often leads to identification of other causes of genitourinary complaints, they said.
Clinical evaluation of patients with pelvic floor dysfunction (PFD) is often limited, both in grading pelvic organ prolapse and identifying the pathologic mechanisms underlying the clinical findings, explained Dr. Patrícia Costa, from the department of radiology at the Hospital Pedro Hispano, Porto, and colleagues. But identification of the underlying pathologic defects can help determine the specific therapeutic approach, which probably results in better outcomes because surgical repair of only one compartment may result in increased dysfunction of the other also-damaged compartments.
"Radiologists should make an effort to answer the clinician's questions, in order to achieve a targeted therapeutic approach," they noted in an e-poster that received a cum laude award from the judges at ECR 2019. "MRI is still able to objectively assess pelvic floor disorders in a noninvasive fashion."
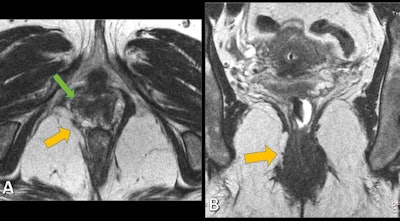 Static axial (A) and coronal (B) T2-weighted MR images allow the identification of structural defects, as disruption of right puborectalis muscle (yellow arrows) and loss of H-shaped vagina on the right side (green arrow). Images courtesy of Dr. Patrícia Costa. © Hospital Pedro Hispano, Hospital Pedro Hispano - Matosinhos/PT.
Static axial (A) and coronal (B) T2-weighted MR images allow the identification of structural defects, as disruption of right puborectalis muscle (yellow arrows) and loss of H-shaped vagina on the right side (green arrow). Images courtesy of Dr. Patrícia Costa. © Hospital Pedro Hispano, Hospital Pedro Hispano - Matosinhos/PT.Quality-of-life impairment
PFD covers a wide spectrum of functional conditions that result from abnormalities of the pelvic floor's supporting structures. The conditions are associated with great impairment of quality of life because they can cause stress urinary incontinence, fecal incontinence, constipation, difficulty in voiding, chronic pain, pelvic organ prolapse, sense of pressure, and sexual dysfunction.
Pelvic floor disorders affect approximately half of women older than 50. The aging of the population has led to an increasing incidence of PFD, representing a great burden in medical care, the authors added.
Against this background, they sought to review the MRI findings of PFD, provide correlation between MRI and clinical findings in patients with PFD, and establish the advantages of a structured MRI evaluation in the assessment of patients with suspected PFD
Treatment of PFD is complex and often involves surgical repair, but surgical options differ according to the underlying defect. Patients with PFD often present with abnormalities in multiple pelvic floor compartments, leading to unsatisfactory results, with postoperative recurrence rates as high as 30% in population-based studies, the group explained.
"As physical and clinical examination have obvious limitations in the evaluation of defects in the anatomic structures and often result in misidentification of the compartments involved, imaging evaluation prior to the surgical repair has been of increasing importance. ... The way pelvic floor MRI is performed and reported by radiologists is still poorly standardized, which led a panel of radiologists with expertise in pelvic floor imaging to create the joint recommendations of the [European Society of Urogenital Radiology (ESUR) and European Society of Gastrointestinal and Abdominal Radiology (ESCAR)] Pelvic Floor Working Group," they wrote.
Recommended protocols
Static and dynamic MRI sequences should be used, and T2-weighted images are recommended for both due to its greater anatomic detail (see table). T1-weighted images should complement the examination whenever a pelvic lesion is detected, the investigators added.
| Recommended MRI protocols | |||
| Plane | Sequence | Technique | |
| Static 2D MRI sequences | |||
| Sagittal | T2-weighted imaging | Turbo/fast spin echo | |
| Transverse | T2-weighted imaging | Turbo/fast spin echo | |
| Coronal | T2-weighted imaging | Turbo/fast spin echo | |
| Dynamic MRI sequences | |||
| Squeezing | Sagittal | T2-weighted imaging | Gradient echo/fast field echo |
| Straining | Sagittal | T2-weighted imaging | Gradient echo/fast field echo |
| Transverse (optional) | T2-weighted imaging | Gradient echo/fast field echo | |
| Coronal (optional) | T2-weighted imaging | Gradient echo/fast field echo | |
| MRI defecography | |||
| Sagittal | T2-weighted imaging | Gradient echo/fast field echo | |
| Coronal (optional) | T2-weighted imaging | Gradient echo/fast field echo | |
Static images lead to detection and classification of structural abnormalities, including defects in the pelvic floor anatomy, supporting structures, and anal sphincter complex. Dynamic images (during squeezing, straining, and defecation) can detect functional abnormalities that are assessed by metric measurements of the three compartments. No oral or intravenous contrast is necessary, according to the researchers.
To view the full e-poster and a wide range of clinical images, go to the group's exhibit in the Electronic Presentation Online System (EPOS) from ECR 2019.
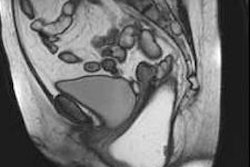
Editor's note: The image used to introduce this article on our homepage is an MRI scan obtained during straining and evacuation. A large anterior rectocele develops, associated with descent of the posterior pelvic floor. Courtesy of Dr. Francesca Maccioni, Sapienza University of Rome. Originally published in ECR Today on 4 March 2011.