The German Radiological Society's uroradiology and genitourinary diagnostics working group has devised a new certification program for multiparametric MRI of the prostate. In a question-and-answer interview, Prof. Matthias Röthke, chairman of the board for the German Radiological Society's Uroradiology and Genitourinary Diagnostics Working Group (AG-URO, DRG), explains about the rationale behind the scheme and how to tap the potential benefits of the emerging technique.
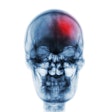
Prostate cancer is the most common cancer in men. Which methods and aids are available for the diagnosis of prostate cancer?
Röthke: Prostate cancer screening comprises the detection of the laboratory parameter prostate specific antigen (PSA) and a digital palpation of the prostate, which is performed transrectally, and usually is followed by transrectal ultrasound (TRUS), which assesses prostate morphology.
 Prof. Matthias Röthke.
Prof. Matthias Röthke.In addition to this established method, more recent methods are available, such as functional ultrasound examinations with elastography and contrast agents, and, of course, multiparametric MRI, which has received extensive scientific evaluation over the past decade in terms of its diagnostic quality.
What is the significance of a prostate biopsy?
As with many other cancers, a conspicuous finding must be clarified histologically in order to be able to initiate adequate therapeutic measures. In the prostate, a systematic biopsy is performed in which, under TRUS guidance, usually two histological samples are taken from the sextants of the prostate.
What exactly can a multiparametric MRI scan do?
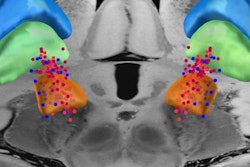
It offers two key benefits. First, it can pinpoint the definitively malignant lesions in the prostate, allowing them to be biopsied and assigned according to the prostate imaging reporting and data system (PI-RADS). This works in a similar way to the BI-RADS classification for breast MR: the higher the PI-RADS score, the greater the likelihood of significant prostate cancer. The question as to whether a targeted biopsy of suspicious lesions alone is sufficient must be clarified conclusively. These days, as a rule, in addition to the targeted biopsy of the conspicuous findings, a systematic biopsy is also performed.
The second major advantage of multiparametric MRI is that it has a very high negative predictive value of around 95%. It can therefore help to avoid unnecessary biopsies, for example, in men who have a PSA increase due to prostate irritation, e.g., prostatitis.
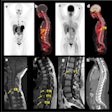
For which indications is multiparametric MRI used?
Currently, multiparametric MRI is used primarily in men, where a systematic TRUS-guided biopsy was unremarkable but the prostate continues to show a suspicious clinical course, such as a further increase in PSA. Current studies, including those from the New England Journal of Medicine, suggest if clinically suspected, multiparametric MRI should be performed prebiopsy to either identify a suitable target for biopsy or directly exclude it. We can thus prevent possible overtreatment as we regularly detect low-grade carcinomas, i.e., carcinomas with a Gleason score of 6, or in the newer pathological classification grade I.
In current diagnostic practice sometimes a not-very-suspicious area is described with a PI-RADS score of 4 or 5, which is then biopsied and the pathological report describes a prostate carcinoma with a Gleason score of 6. This is not a good result for either radiologists or urologists, as we know from large studies that life expectancy is not significantly reduced by these low-grade carcinomas. Instead, however, many patients for whom active surveillance is actually sufficient, will, after a few years, opt for more radical therapies, leading not only to organic function loss, but also to significant healthcare costs.
We also know that patients with a cancer diagnosis, including patients diagnosed with low-grade prostate cancer and who are only monitored but not treated, have an increased suicide rate.
What role does multiparametric MRI play in the decision for or against a prostate biopsy?
This depends on how progressive the process is. In the guidelines, which always follow the current state of research, a biopsy is recommended if a suspicious or highly visible area with a PI-RADS score of 4 or 5 is detected. Whether a biopsy, specifically a first biopsy, is not performed in the case of a negative multiparametric MRI scan depends on the treating or supervising physicians. I assume that in the near future no biopsy will be carried out if the findings are inconspicuous after a quality-assured and standardized multiparametric MRI examination. At the moment, nobody can say exactly when this will be reflected in the guidelines. First, a positive assessment by the Joint Federal Committee and clarification of reimbursement issues by the statutory health insurers are desirable.
What are the requirements for radiologists performing multiparametric MRI examination of the prostate and what skills are required for this?
Here it is important to distinguish between the technical part of carrying out the examination and the diagnosis. Technical implementation is not a trivial matter due to its complex functional elements. These include diffusion-weighted imaging (DWI) and a perfusion study using contrast agent dynamics. Particularly for DWI, a modern MR scanner with the appropriate gradient strengths is necessary in order to achieve reasonable results.
The field strength is also important: 3-tesla allows faster examinations due to the better signal-to-noise ratio (SNR) or successful performance in obese patients. With regard to the technical parameters, the DRG's Uroradiology and Genitourinary Diagnostics Working Group has prepared and published a guideline that can serve as a technical guide for performing MR prostatography. Also important is the evaluation of the multiparametric MR scan of the prostate: This requires good training and regular exercise. Due to constantly growing demand, there are now various training courses and symposia throughout Germany.
Incidentally, the working group will also offer a basic and a special course on multiparametric MRI at the 100th German Radiology Congress in 2019.
What motivated you to set up a certification program for multiparametric MRI?
The results of the sometimes very high level studies on multiparametric MRI have led to a growing demand from urologists. In multiparametric MRI's application, however, it has been shown that inadequately trained radiologists, who may not even have the necessary technical equipment, overlook carcinomas or detect false-positive findings and also do not use the standardized PI-RADS system for reporting findings. We therefore see it as our task to guarantee quality standards for the professional and technical implementation of this specific examination method via special certification.
What certificates do you offer and how can one apply?
We offer two certificates: a Q1 certificate and a Q2 certificate. Both can be applied for after becoming a radiology specialist. Initial experiences with multiparametric MRI may have already accumulated naturally of course through specialist training. The Q1 certificate is aimed at colleagues who primarily want to carry out diagnostic MRI examinations of the prostate gland. The Q2 certificate is in principle intended for those who work at large centers, in, for example, biopsy planning, staging, post-therapy monitoring, and recurrence diagnostics.
The introduction of the multiparametric MRI prostate special certification was decided at the 99th national radiology congress in May 2018. In the meantime, the requirements for certification and the exact course of the certification process have been defined. The relevant application documents can be viewed and downloaded from the homepage of the DRG's Uroradiology and Genitourinary Diagnostics Working Group.
How do you assess the demand for the new certification?
Due to the increasing demand for prostate MRI across different disciplines, I am optimistic and assume that we will have the first 100 colleagues certified by the end of 2019.
Editor's note: This is an edited version of a translation of an article published in German online by the German Radiological Society (DRG, Deutsche Röntgengesellschaft). To read the original version, click here.