Not offering breast screening to women at lower risk of cancer could improve the cost-effectiveness of screening programs, reduce overdiagnosis, and maintain most of the benefits of screening, according to U.K. research published online on 5 July by JAMA Oncology.
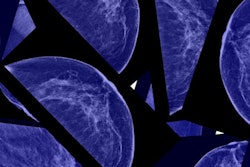
The U.K. Breast Cancer Screening Programme invites all women ages 50 to 69 for two-view digital mammography every three years, but this age-based, "one-size-fits-all" screening approach does not take into account individual variation in risk, noted a team led by Nora Pashayan, PhD, a clinical reader in applied health research at University College London.
 Nora Pashayan, PhD, from London.
Nora Pashayan, PhD, from London."The trade-offs of benefits and harms vary by the risk threshold we use to define the low-risk group," Pashayan told AuntMinnieEurope.com. "There is value judgment in defining the low-risk group -- how many overdiagnoses we are prepared to accept to prevent one death from breast cancer. Different women will have different preferences."
By looking at how cost and quality-adjusted life years (QALYs), a measure of health outcomes, varied by risk threshold, the researchers found that the more lower-risk women are screened, the more the cost of the screening program increases without further gains in QALYs. Sparing women at lower risk would lead to the same benefits of screening at the population level and reduce costs, they stated.
Risk-stratified screening
The research team addressed a central question: Can risk-stratified screening for breast cancer improve the cost-effectiveness and benefit-to-harm ratio of screening programs?
The researchers created a statistical model of a hypothetical cohort of 364,500 women in the U.K., starting at age 50 with follow-up to age 85, using data from the Independent U.K. Panel on Breast Cancer Screening and risk distribution based on risk profile. The analysis was undertaken from the National Health Service (NHS) perspective (JAMA Oncol, 5 July 2018).
The researchers first compared age-based screening to no screening at all. Among the women who were screened, they found 1,913 fewer deaths from breast cancer and 3,819 fewer overdiagnosed breast cancers in the age-based screened cohort than in the unscreened cohort. Age-based screening resulted in 1,916 QALYs at an additional cost of 41.9 million pounds (47.4 million euros).
They then compared the same metrics in hypothetical programs that directed mammography screening to women at different thresholds of risk -- for example, 10% representing women at very low risk and 90% representing women at high risk. They found that as the risk threshold was lowered, the incremental cost of the program increased linearly compared with no screening, with no additional QALYs gained below the 35th percentile risk threshold, the authors explained.
Of the three screening scenarios, the risk-stratified scenario with risk threshold at the 70th percentile had the highest net monetary benefit, at a willingness to pay of 20,000 pounds (22,603 euros) per QALY gained. Compared with age-based screening, risk-stratified screening at the 32nd percentile versus 70th percentile risk threshold would cost 20,066 pounds (22,677 euros) versus 537,985 pounds (607,998 euros) less, would have 26.7% versus 71.4% fewer overdiagnoses, and would avert 2.9% versus 9.6% fewer breast cancer deaths, respectively.
| Comparison of risk-based breast screening at different risk thresholds | |||
| Age-based screening | Risk-based screening at 32nd percentile threshold | Risk-based screening at 70th percentile threshold | |
| No. of breast cancers detected | 875 | 834 | 776 |
| No. of breast cancer deaths | 239 | 246 | 262 |
| No. of overdiagnoses | 105 | 77 | 30 |
| Cost of program | 6.37 million euros | 6.34 million euros | 5.76 million euros |
| QALYs | 128,892 | 129,342 | 129,335 |
Boosting cost-effectiveness
The cost-effectiveness and the benefit-to-harm ratio of the NHS Breast Screening Programme could be improved by adopting a risk-stratified screening strategy, according to Pashayan and colleagues.
"The optimal risk threshold for risk-stratified screening depends on the acceptable trade-off between improving cost-effectiveness and maximizing benefits and minimizing harms of screening," they noted. "Not offering screening to women in the lower tertile of the risk distribution would improve the cost-effectiveness of the breast screening program, reduce overdiagnosis while maintaining the benefits of screening."
In an accompanying editorial, Megan Roberts, PhD, a cancer prevention fellow in the Behavioral Research Program within the Division of Cancer Control and Population Sciences at the U.S. National Cancer Institute in Rockville, Maryland, noted that one of the authors' key findings was that risk-targeted screening at the 70th percentile risk cutoff would cost 537,985 pounds (607,998 euros) less than age-based screening, with 71% fewer overdiagnoses.
"When screening was targeted to women with a risk threshold of 70% or less, the number of cancer deaths avoided through screening was less than the number of overdiagnoses," she wrote. "These findings suggest that a risk-stratified screening program in which those with low risk are not offered breast cancer screening would be more cost-effective and result in fewer overdiagnoses, though it would avert 9.6% fewer breast cancer deaths than age-based screening."
Roberts thinks the authors have provided evidence for a promising approach to precision screening in breast cancer, but an important question remains: Are we ready to translate precision screening for breast cancer that incorporates risk to the population level?
There's an urgent need for additional implementation research about precision screening approaches across patient, clinician, and health system levels, and as prevention becomes increasingly more precise, it is essential to address these issues such that the promise of precision screening can be achieved, she concluded.
Future plans
Pashayan and her colleagues intend to continue their risk-stratified screening work and to study the risk threshold that is acceptable to women. Robust data are needed to evaluate fully risk-tailored screening, and policymakers, health professionals, the public, and the scientific community have to work together to enable provision of screening program that can do more good than harm at an affordable cost, they asserted.
Through a project funded by a charitable group called Breast Cancer Now, they are evaluating whether and how breast cancer progression and mammogram sensitivity vary by risk.
"This is to study the benefit-to-harm ratio and cost-effectiveness of risk-tailored screening for breast cancer, where the age of start of screening and the frequency of screening could be varied according to risk level," Pashayan explained. "In international collaboration with colleagues in Canada, as part of the PERSPECTIVE I&I [Personalized Risk Assessment for Prevention and Early Detection of Breast Cancer: Integration and Implementation] study, we are looking into the prerequisites for implementation of risk-stratified screening for breast cancer."