Shear-wave elastography (SWE) differentiates malignant from benign breast lesions with high accuracy and a very high negative predictive value, according to Israeli researchers. In addition, the technique is not affected by the immediate density of the tissues surrounding the lesion or the depth of the lesion
The group, led by Dr. Tamar Sella from the department of radiology at Hadassah-Hebrew University Medical in Jerusalem, measured SWE in nearly 350 breast masses undergoing biopsy to evaluate how anatomic factors affect performance. The team found SWE correctly defined benign lesions in 93% of cases and malignant lesions in almost 80% of cases.
Using SWE
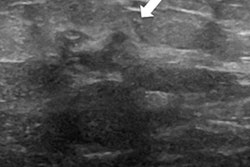
SWE is a form of elastography, a measurement of tissue elasticity in which external stress is induced by ultrasound beams perturbing tissue using an acoustic radiation force, which applies pressure in the direction of beam propagation. This results in transverse shear waves that propagate in the surrounding tissue in sort of a ripple effect like throwing a stone into the water, according to Sella.
Elasticity and propagation transverse shear waves are directly linked; the stiffer the lesion is, the faster these waves develop as measured in higher kilopascals (kPa).
"We know that different tissues have different inherent elasticity properties," she told delegates at ECR 2018. "And we know that in regular fatty breast tissue there is very low elasticity as compared with glandular tissue, which has a higher, inherent, internal elasticity property; and fibrous tissue, which has a higher elasticity. The waves travel faster through the stiffer tissue."
Breast cancer elasticity ranges from very low to very high, with higher elasticity in benign lesions. SWE measures not inside the lesion itself but rather the waves that transverse the tissue surrounding the lesion. Because each lesion has different inherent properties, do those properties affect SWE? That's precisely what the researchers sought to find out.
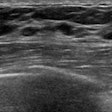
Their retrospective analysis included 349 consecutive lesions, with each patient undergoing ultrasound-guided biopsy with SWE performed just before the biopsy. Sella and colleagues categorized the lesions into dense or fatty breast tissue, as well as by lesion depth (superficial, midbreast, or deep). They used the Emax parameter, which is the fastest or the highest parameter, as a parameter for analysis.
They used receiver operating characteristic (ROC) curve analysis to define the optimal cutoff point at 59.4 kPa, resulting in a sensitivity of 90.1% and a specificity of 84.9% with an area under the curve (AUC) of 0.929. SWE also demonstrated a positive predictive value (PPV) of 78.1% and a negative predictive value (NPV) of 93.4%.
Biopsy revealed 218 benign lesions and 131 malignant lesions. Using the defined cutoff point, SWE correctly defined benign lesions in 93% of cases and malignant lesions in almost 80% of cases.
When looking at dense and fatty breast tissue, the researchers found no difference regarding elasticity or elastography measurements. Also, clinical performance remained the same with more than 90% of benign lesions defined as benign, and between 70% and 87% of malignant lesions defined as malignant. SWE identified 58 out of 82 (70%) of malignant lesions in dense breasts and 60 out of 69 (87%) of malignant lesions in fatty breasts.
"When trying to determine the optimal cutoff point for each subgroup, there was no difference between optimal cutoff points with the same parameters and specificities," Sella said.
The researchers also turned their attention to lesion depth, wondering whether proximity to the skin (superficial) or proximity to the chest wall (deep) would affect clinical analysis. They identified 79 superficial, 137 midbreast, and 117 deep lesions with no differences among the three groups. Again, SWE's ability to identify benign and malignant lesions remained the same -- identifying benign lesions as benign in more than 90% of cases in all three depths and identifying malignant lesions as malignant in more than 70% in all cases.
"Shear-wave elastography differentiates malignant from benign lesions with high accuracy and specifically has a very high negative predictive value," Sella concluded.