A health IT project conceived in Liverpool, U.K., that allows sharing of a pool of radiology trainees working in a call center to cover multiple departments is showing initial signs of success. Fresh information on the scheme was presented at ECR 2015.
In the U.K., the end of the national PACS project has led to procurement of local PACS. In Merseyside, a region in northwest England that includes the city of Liverpool, there was a particular issue with very high levels of patient movement, related to multiple providers and movements for specialist care.
"In our procurement, there was a strong clinical need to avoid the high levels of image transfer and repeat exams," noted Dr. Peter Rowlands, consultant radiologist and clinical lead for PACS procurement at the Royal Liverpool and Broadgreen University Hospitals National Health Service Trust (RLBUHT), and colleagues in an ECR 2015 e-poster. "We procured a PACS (Carestream Health) that allowed multiple PACS to behave as a single virtual PACS and allow display of prior exams from multiple sites."
The main objective was to ensure compliance with the European Working Time Directive (EWTD), thereby improving work/life balance and health, and reducing mistakes related to tiredness. Other goals were to allow collaborative working to aid reporting by peer support, to reduce the requirement for sole working, and to cut the need for compensatory rest and lost training days. Overall, these aims have been achieved, they stated.
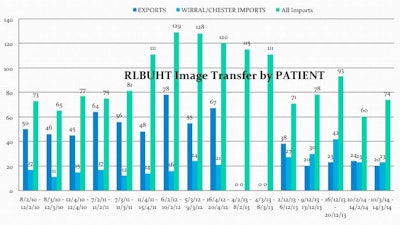
Image transfer volumes before and after the single virtual PACS. Source: Radiology Department, Royal Liverpool University Hospital.
Merseyside is a small but complex health region, having seven acute district hospitals, as well as specialist hospitals for neurology, chest/cardiac, obstetrics/gynecology, pediatrics, and cancer. Until summer 2013, individual hospitals had separate PACS, and image sharing was via an email-like image exchange portal or by CDs. On-call, out-of-hours radiology service was provided by specialist registrars (i.e., residents) based at each hospital, and the numbers varied from five to 10. Several full-time posts at each institution were devoted to image transfer for patient transfers, or for multidisciplinary meetings (MDTs), explained the authors.
Given the large number of National Health Service (NHS) trusts within the region, many patients have to attend different hospital sites for certain types of treatment or services, and sometimes patients have had studies carried out where there was no specialist available to interpret the results. Queues were common, and sometimes downloading had to be an overnight event, rather than being done in real-time, and this meant the sharing of patient notes and images between the hospital sites was slow and costly.
To address the problem, Rowlands et al began a pilot project in early 2014, where two acute sites combined trainees into one out-of-hours rota. There was a virtual call center in which the on-call trainee was based. A third site joined in mid-2014, followed by a fourth in early 2015. The call center has developed into a physical entity, and the other three acute sites are due to be added by August 2015.
A single RIS worklist is used to show unreported studies from all sites, and reporting can also be done within the PACS, which is appropriate for the non-Carestream sites, they continued. Two of the hospitals had procured or maintained PACS from other vendors, but a Caresteam "agent" allows non-Carestream sites to behave as if they are on the single virtual PACS. Review and reporting of images from any of the Carestream sites are performed in real time.
Additionally, they have made four practical adjustments:
- Protocols for radiographers to perform contrast injections without a resident radiologist being present.
- An Internet protocol (IP) network, mobile phone system, as mobile phone signal was very poor at one site.
- Access to ultrasound lists performed by on-site radiologists/sonographers.
- Increased level of consultant support for mentoring and review of cases.
No critical incident or patient harm has occurred, according to the authors. There have been several minor incidents of failure to communicate with a trainee, but these were resolved with input from a senior radiologist/consultant, and compliance with the EWTD has been achieved. An urgent ultrasound exam was required when a trainee was not in the hospital, and it had to be performed by a consultant. There was some minor downtime of the virtual PACS. Also, a consultant from a nontrainee department reviewed cases from home using teleradiology.
The new setup is almost universally popular with trainees and less educational time has been missed, they stated. It has led to a reduction in image transfer workload following shared virtual PACS, and furthermore, implementation has been neutral in terms of cost.
"The pilot and then the addition of the third site have been performed almost without clinical incident," the authors noted. "With additional departments there will be peer support by a team of trainees."
There are downsides, however, including the larger rota (hence greater administrative workload), change in clinician mindset moving from resident to remote opinion, staff being busier when covering more than one organization, handover more difficult, more consultant input in reviewing cases, and loss of "pair of hands" for intervention.