The ingestion of fish bones and other foreign bodies and their impaction in the upper aerodigestive tract is a common emergency, and radiologists must keep aware of the range of pitfalls in interpretation that can affect patient management, according to prize-winning research from Spain.
"Frequently laryngeal cartilages, with their variable pattern of ossification, create a diagnostic problem on the assessment of laryngeal foreign bodies," noted lead author Dr. Alba Castán Senar, from the department of radiology at Miguel Servet University Hospital in Zaragoza. "The radiologist must be familiar with these false images on the soft-tissue lateral neck x-ray."
In an e-poster that received a Cum Laude award at last month's RSNA 2015 meeting in Chicago, Castán Senar and colleagues presented a practical and timely chart about how best to handle pharyngoesophageal foreign bodies (see figure).
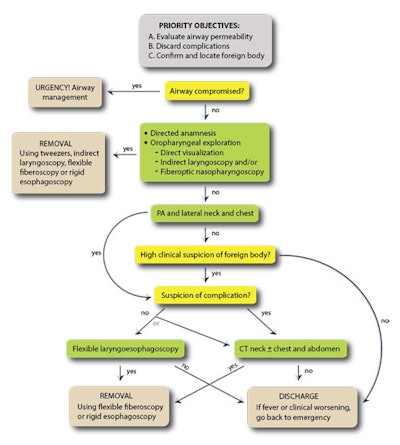 Pharyngoesophageal foreign bodies: diagnostic and therapeutic algorithm. Source: Dr. Alba Castán Senar et al, Miguel Servet University Hospital, Zaragoza, presented at RSNA 2015.
Pharyngoesophageal foreign bodies: diagnostic and therapeutic algorithm. Source: Dr. Alba Castán Senar et al, Miguel Servet University Hospital, Zaragoza, presented at RSNA 2015.Visualization of an ingested foreign body depends on its radiodensity and location. Previous research has found that lateral neck radiographs had a sensitivity of more than 57% and a specificity of around 76%, with a high detection rate (72.5%) when foreign bodies were lodged in the hypopharynx and cervical esophagus, but the detection rate was poor in the oropharynx, they explained. Also, existence of prevertebral soft-tissue swelling is an indirect sign of foreign body presence; this is particularly important because many fish and meat-bones are radiolucent.
Among the foreign body mimics are laryngeal cartilage ossification, including the superior margin of the cricoid lamina, vertical ossification of posterior margin of cricoid lamina, superior cornu of thyroid cartilage, arytenoid cartilage, and triticeous cartilage in lateral thyrohyoid membrane. Furthermore, two areas in the cricoid are liable to be confused with a foreign body: superior tip of the cricoid lamina and vertical ossification of posterior margin of cricoid lamina.
CT can show that the calcification corresponds to the ossified superior margin of the cricoid lamina. Also, CT can show the calcification corresponds to vertical ossification of the posterior margin of cricoid lamina. Sometimes, the ossified arytenoids and the superior cornus of the thyroid cartilage may be mistaken for foreign bodies, the authors stated.
"Thyroid cartilage calcification/ossification commences at 20 years old. It starts at postero-inferior part of lamina and inferior cornua. It progresses upwards and anteriorly, so it is unusual to see isolated superior lamina or superior cornua ossification. Eventually, the male thyroid cartilage completely ossifies, whereas in females the anterior aspect is left unossified," they wrote. "Arytenoid calcification starts from the base of arytenoids sitting on the upper aspect of the cricoid lamina. When completely calcified, it produces an L-shaped appearance."
Triticeous cartilage calcification is usually asymptomatic, and occurs in 29% of men and 22% of women. It can present as "eagle-like" syndrome, and this cartilage localizes in the posterior thyrohyoid membrane, where it can mimic a foreign body.
Carotid atheromas can lead to errors in radiographic interpretation, suggesting a foreign body is located in regional soft tissues, and anteroposterior cervical radiographs are helpful for a differential diagnosis. Carotid atheromas are mostly circular when they are small and irregular and linear when they have a larger size, Castán Senar et al continued.
"Epiglottis is an elastic cartilage. Although textbooks assert that elastic cartilage shows no tendency to calcify or ossify, currently some cases of calcification of the epiglottis have been reported in the literature," they wrote. "Calcium deposits in the epiglottis have a tendency to increase with age, and might be a very rare cause of abnormal epiglottic movement pattern and dysphagia."
Between 80% and 90% of pharyngoesophageal foreign bodies progress through the digestive tract spontaneously, and in adults, the most common foreign bodies are fish bones and chicken bones. In the oropharynx, they are located in the palatine tonsils (most common), tongue base, valleculae, and lateral pharyngeal wall. Diagnosis is by direct laryngoscopy. In the hypopharynx, diagnosis is by indirect laryngoscopy and fiberoptic pharyngoscopy, lateral neck radiograph, and cervical CT.
In the esophagus, the typical locations are areas of pathological or physiological stenosis, medial esophagus (protrusion of the aortic arch and left main bronchus, at D4 level), lower esophageal sphincter, and cricopharyngeal muscle (upper esophageal sphincter), the most common area of impaction being at C6 level. Diagnosis is by indirect laryngoscopy, retention of saliva in pyriform sinuses (indirect sign), neck and chest x-ray, cervical and thoracic CT, and flexible laryngoesophagoscopy, according to the authors.
"For evaluation of patients with suspected pharyngoesophageal foreign bodies, an anteroposterior and lateral neck and chest should be obtained. Lateral and anteroposterior radiographs are important because some foreign bodies, especially those of discoid shape, sometimes cannot be identified only in one projection," they noted, adding that if radiography is not conclusive but there is a strong clinical suspicion, a neck CT scan will be useful to confirm the existence and location of the foreign body and allows assessment of the presence of complications.
Furthermore, in older patients, food boluses also present as foreign bodies and tend to lodge at the level of the cervical esophagus, causing aphagia and drooling of saliva, the authors wrote. Radiographic evaluation is useful to detect any associated complications, such as cervical or mediastinal air from perforation, but food boluses are radiolucent and not readily visualized on plain radiographs. Radiographs can reveal cervical esophageal swelling and an air-fluid level, which are indirect signs of a food bolus. After the food impaction is treated, an esophagram should be completed to look for abnormal esophageal strictures or esophageal motor disorders, they concluded.