
Since 1989, it has been standard practice in the U.K. to estimate mean glandular dose (MGD) -- the dose received by glandular tissue in the breast during mammography -- using conversion factors applied to the incident air kerma (kinetic energy released per unit mass).
 David Dance, Consultant Physicist at the National Coordinating Center for the Physics of Mammography (NCCPM) in the U.K.
David Dance, Consultant Physicist at the National Coordinating Center for the Physics of Mammography (NCCPM) in the U.K.The original factors were calculated by David Dance, who now works at the National Coordinating Center for the Physics of Mammography (NCCPM) in Guildford, U.K. and have been adopted for use in Europe and by the International Atomic Energy Agency (IAEA).
Now, MGD resulting from contrast-enhanced digital mammography (CEDM), an up-and-coming imaging technique, can also be estimated using new factors calculated by Dance and NCCPM head Ken Young. The factors will enable CEDM to be compared with more established mammography techniques and for imaging protocols to be optimized according to dose (Physics in Medicine and Biology, 4 April 2014, Vol. 59:9, pp. 2127-2137).
"Previous tabulations of these conversion factors do not cover the relatively high-energy spectra used for CEDM and prior to our publication, no data were readily available to facilitate the estimation of breast dose for this examination," said Dance, who is also a consultant physicist at the Royal Surrey County Hospital and a visiting professor at the University of Surrey.
Interest in CEDM
The study was motivated by increasing interest in CEDM, which uses higher-energy x-ray spectra than conventional mammography to image the abnormal vasculature associated with tumors, using an injected iodine contrast agent and image subtraction. While research into its efficacy is still ongoing, it may offer a lower-cost, more convenient alternative to contrast MRI.
Mammography dosimetry protocols use three factors to convert incident air kerma to MGD. The g-factor calculates MGD for a breast with an equal mix of adipose and glandular tissue; the s-factor corrects MGD for x-ray spectra produced by different target/filter combinations in the x-ray tube; and the c-factor corrects for varying breast glandularity.
Dance and Young applied the same approach as in previous studies, using the same Monte Carlo model to calculate MGD, from which the conversion factors could be derived. Breast thicknesses from 20 to 110 mm were simulated, and with only one CEDM system on the market and no CEDM energy spectra in the literature, the researchers used spectra provided by manufacturers.
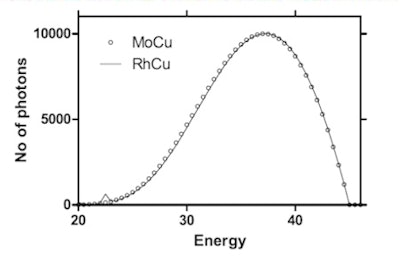 Simulated CEDM spectra for the target-filter pairs are dominated by bremsstrahlung radiation. Once normalized and matched for HVL and tube voltage, they were very similar to one another, effectively setting the s-factor to one.
Simulated CEDM spectra for the target-filter pairs are dominated by bremsstrahlung radiation. Once normalized and matched for HVL and tube voltage, they were very similar to one another, effectively setting the s-factor to one."We surveyed all x-ray manufacturers and used spectra that covered the range being considered for CEDM," Young said. They simulated spectra for molybdenum, rhodium, and tungsten targets, each with 0.30 mm of copper filtration, and with tube voltages varying in 1 kV steps between 40 kV and 50 kV. A total of 53 spectra were simulated for the three target-filter pairings.
Once matched for HVL (half value layer, a measure of beam penetration) and tube voltage, the spectra for the different targets proved highly similar. The similarities arise as element-specific radiation peaks are removed or markedly reduced by the copper filters, leaving bremsstrahlung-dominated spectra that are closely matched. Consequently, the s-factor is effectively set to a value of one, eliminating it from CEDM dose estimations.
','dvPres', 'clsTopBtn', 'true' );" >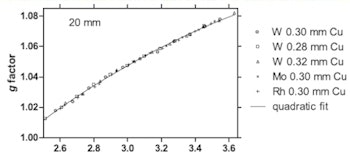
Plotting the calculated g-factors for all spectra against HVL, quadratic curves for each breast thickness provided close matches. Using these fits, Dance and Young generated a table of factors for different HVL values and breast thicknesses. A similar fitting strategy was used for the c-factor, and values were tabulated for a range of breast thicknesses, HVLs, and breast glandularity.
Incorporation of the new factors into mammography protocols in the U.K., the rest of Europe, and worldwide will only occur when the protocols undergo broader, formal revisions. In the meantime, Dance and Young plan to inform the relevant bodies of the availability of the data.
To supplement their work, Dance and Young have also calculated conversion factors that will enable CEDM dose estimation using polymethyl methacrylate (PMMA) phantoms that simulate typical breasts. The factors will be made available through the NCCPM website in the first instance. Like those calculated in the study, they will enable comparison of different mammography techniques and aid quality control programs comparing doses between and within mammography centers.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.



















