Diffuse optical tomography can characterize breast lesions noninvasively with nonionizing near-infrared light, and by combining a tomography scan with mammography images, this technology may be able to differentiate malignant from benign breast tumors, according to research from the U.S. and France.
A group from Massachusetts General Hospital's Martinos Center for Biomedical Imaging, in collaboration with Philips Research Medisys in Paris, has developed and validated a method for fusing tomographic optical images with 2D digital mammography images. The resulting joint optical/x-ray image reconstruction creates improved spatial resolution in the optical images and enables robust optical property estimation. The research team believes this achievement represents an important step in the development of a portable, low-cost diffuse optical tomography breast scanner that can be used in conjunction with all digital mammography systems.
Principal investigator Qianqian Fang, PhD, an assistant professor of radiology, and colleagues, previously investigated the integration of diffuse optical tomography with 3D digital breast tomosynthesis (DBT) images for a patient cohort of 450 women, using a combined diffuse optical tomography/DBT system. Their latest research examined a subset of 67 women who had been diagnosed with a breast lesion 8 mm or greater in one breast, and had both a valid diffuse optical tomography scan and an independent bilateral mediolateral-oblique view 2D diagnostic mammogram taken within a 90 day interval.
The team proposed a technique to jointly utilize the breast tissue anatomy and the functional optical assessment obtained from two separate breast compressions. The key to this approach is an effective image registration algorithm that matches the breast contour lines extracted from the mammogram and the middle-axial cross-section of the breast surface from the DBT scan (which is coregistered with the diffuse optical tomography data) (Journal of Biomedical Optics, 11 August 2015).
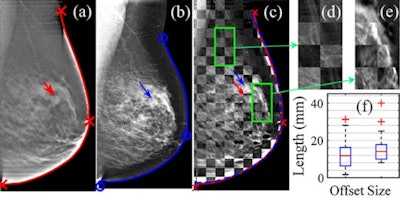 Demonstration of the registration algorithm for matching the breast contour lines (red/blue lines) from DBT (a) and 2D mammography (b) scans. After matching the breast contours, the internal tissue anatomy shows good alignment in the checker-box overlay (c) of the two images. For all 67 lesion cases, the mean tumor offset generated from the registration was 12.7 ± 0.9 mm, as shown in the box plot in (f). Image credit: Characterizing breast lesions through robust multimodal data fusion using independent diffuse optical and x-ray breast imaging, 2015 Bin Deng et al J. Biomed. Opt.
Demonstration of the registration algorithm for matching the breast contour lines (red/blue lines) from DBT (a) and 2D mammography (b) scans. After matching the breast contours, the internal tissue anatomy shows good alignment in the checker-box overlay (c) of the two images. For all 67 lesion cases, the mean tumor offset generated from the registration was 12.7 ± 0.9 mm, as shown in the box plot in (f). Image credit: Characterizing breast lesions through robust multimodal data fusion using independent diffuse optical and x-ray breast imaging, 2015 Bin Deng et al J. Biomed. Opt.Fang explained the fusion process: "The image fusion process is achieved in two steps. First, we try to align the x-ray mammogram to the optical probe space, a process that is particularly important for this study. Unlike our previous studies where the optical data were obtained in spatial coregistration with the x-ray scans, in this study we aim to combine separately acquired optical and x-ray images from independent systems. Because of the independent breast compressions, it is necessary to first match the two imaging fields-of-view before using the information together."
Once the mapping between the mammogram and the optical data space is determined, the anatomical information in the mammogram is transformed into the optical space and converted into a "soft constraint" to guide optical image reconstruction. In other words, the optical image reconstruction not only considers matching the measured optical data, but is also aware of the x-ray intensity similarities across various regions.
"If two areas have similar x-ray intensities, our algorithm 'hints' the image reconstruction to produce similar optical properties where possible," Fang said. "As the output of this process, the reconstructed optical images contain information from both modalities, and have noticeably better spatial details compared to optical reconstructions without anatomical guidance."
For the validation cohort of 67 patients, the technique demonstrated comparable performance to the coregistered DBT-guided diffuse optical tomography. Combining separately acquired optical and x-ray data resulted in statistically significant differentiation between all combinations of adipose, fibroglandular, and malignant tissues in the recovered total hemoglobin concentration images of malignant tumor-bearing breasts.
More importantly, the approach could differentiate malignant lesions from solid benign lesions, as well as from normal tissue, using normalized hemoglobin concentration. A strong correlation was also observed between all lesion hemoglobin concentration values recovered using 2D and DBT-guided approaches.
The authors differentiate their research from other similar studies in these ways:
- The technique simultaneously uses the information acquired from the diffuse optical tomography scan and the mammogram in a single diagnosis.
- The optical breast scanner is designed to mimic standard mammographic compressions to minimize the registration error.
- The focus of the study is part of on-going research to enable robust image fusion with x-ray mammography, thus specifically addressing the need to improve early diagnosis of breast cancer.
"By having the ability to utilize information from separate functional (optical) and structural (x-ray) breast scans, we can enable multimodal breast imaging analysis without the need to replace in-service mammography systems," Fang said. "We hope to develop an optical breast imaging system that can be used side-by-side instead of requiring integration or replacement of in-use digital mammography systems."
The ultimate goal: to provide radiologists with robust functional tissue assessment and help them better differentiate malignant from benign tumors. As a result of this ability, the number of unnecessary biopsies and the number of missed cancers could potentially be reduced.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.