One-view breast tomosynthesis shows higher diagnostic accuracy as compared with two-view digital mammography, helping interpreting radiologists find 10% more cancers, according to a new study from an influential group of researchers in Sweden.
The findings are encouraging, especially since digital mammography can produce "noisy" images due to the intrinsic limitations of using a 2D technology to image a 3D structure, according to lead author Tony Svahn, PhD, of the Malmo University Hospital in Malmo, Sweden, and colleagues.
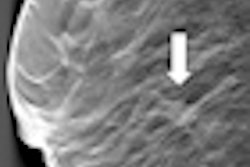
"Two views -- mediolateral oblique and craniocaudal -- can partially compensate for the overlapping anatomical noise [produced by digital mammography], but this depends on the radiologist's ability to mentally fuse the two images," Svahn and colleagues wrote in the British Journal of Radiology (6 June 2012). "Breast tomosynthesis collects two-dimensional projection views over a limited angular range, which allows reconstruction of thin slices of the breast volume."
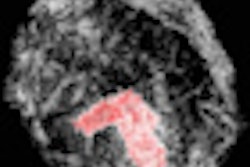
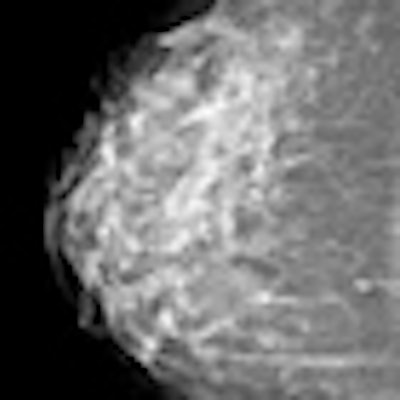
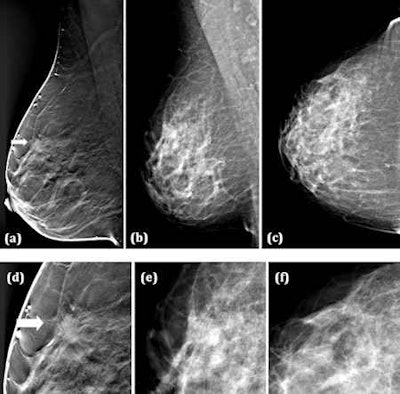 (a) Breast tomosynthesis (BT) mediolateral oblique view (one-view BT), (b) Digital mammography (DM) mediolateral oblique, and (c) DM craniocaudal view (two-view DM), (d-f) close-ups of (a-c). A 49-year-old woman with a 10-mm spiculated invasive tubular carcinoma grade 1. The tumor was detected by 5/5 readers on one-view BT, while on two-view DM (b, c) the tumor was undetected by all the readers. All images courtesy of Tony Svahn, PhD.
(a) Breast tomosynthesis (BT) mediolateral oblique view (one-view BT), (b) Digital mammography (DM) mediolateral oblique, and (c) DM craniocaudal view (two-view DM), (d-f) close-ups of (a-c). A 49-year-old woman with a 10-mm spiculated invasive tubular carcinoma grade 1. The tumor was detected by 5/5 readers on one-view BT, while on two-view DM (b, c) the tumor was undetected by all the readers. All images courtesy of Tony Svahn, PhD.Svahn's team compared radiologists' ability to detect breast cancers using two-view digital mammography and one-view breast tomosynthesis (Mammomat Novation DR and a tomosynthesis prototype based on this device, both Siemens Healthcare). The prototype breast tomosynthesis system delivered about the same average glandular dose as the two-view digital mammography system, they noted.
The study cohort included symptomatic as well as asymptomatic women examined between June 2006 and May 2008, although the case set was enriched with more cancer cases than usually found in the general population. Women with suspicious findings underwent fine-needle or core biopsy, followed by surgery and histopathological analysis. Of the 185 patients (one breast per patient), 89 were shown to have cancer; 95 abnormalities were found in these 89 women.
Five radiologists blinded to whether the images were malignant or benign interpreted the exams, marking all perceived cancers and assigning malignancy ratings to them based on the BI-RADS scale. In terms of breast cancer visibility, the interpreting radiologists stated that in 12 out of the 95 cases cancer was not visible in either digital mammography view, in 21 cases cancer visibility was subtle, and in 62 cases the cancer was clearly visible. Prior to the study, reader radiologists underwent a training session using 30 corresponding breast tomosynthesis and digital mammography cases -- none of which were used in the actual study.
Pathology results showed that of the 95 cancers, 57 (60%) were invasive ductal carcinomas; the second most common type of cancer was invasive lobular carcinoma -- 19 (20%) of the 95 cancers found. In terms of breast cancer visibility, the interpreting radiologists stated that in 12 out of the 95 cases cancer was not visible in either digital mammography view, in 21 cases cancer visibility was subtle, and in 62 cases the cancer was clearly visible.
Svahn and colleagues found that breast tomosynthesis proved more sensitive as compared with digital mammography, even with only one view: An average of 10.4 more breast cancers per reader were found on breast tomosynthesis than on digital mammography. Breast tomosynthesis had a 90% sensitivity rate, versus a 79% rate for digital mammography, and the false-positive average between the two modalities was comparable.
"It is encouraging that breast tomosynthesis performed better than digital mammography even though the radiologists had much less experience in the breast tomosynthesis modality compared with digital mammography, and with only one view available in breast tomosynthesis compared with two views in DM [digital mammography]," Svahn and colleagues stated. "This suggests that with increased experience, and perhaps with the addition of the corresponding ipsilateral digital mammography view, breast tomosynthesis would have performed even better."
Svahn's group acknowledged that adding this second view using breast tomosynthesis would increase the radiation dose by 50%. But the team noted that further improvements in the technology that will address this issue are sure to come.