MRI provides accurate assessment of perianal fistula and can identify associated abscesses with important surgical implications, according to top award-winning research presented at this month's European Society of Gastrointestinal and Abdominal Radiology (ESGAR) annual meeting in Paris.
Simple or low fistula can be treated with fistulotomy, while complex or high fistula requires a staged operation, usually with initial placement of a drainage seton to resolve the acute inflammation followed by subsequent secondary track closure with variable sphincter-preserving options, noted Dr. Mon Ben Chow, medical officer in the department of diagnostic radiology at Khoo Teck Puat Hospital in Singapore. Incision and drainage must be performed to treat any associated abscess to prevent recurrence.
"Postoperatively, MRI is also helpful to differentiate recurrent or residual disease from fibrosis," Chow and colleagues noted. "Radiologists should familiarize themselves with these findings to aid the surgeons in achieving optimal surgical outcomes."
The group's e-poster received the only Magna Cum Laude at the Paris meeting. It was the most popular exhibit with 484 views, and it achieved a rating of 8.15 out of 10.
Anatomy know-how
Perianal fistula is a common condition encountered daily in a busy colorectal practice, and while most uncomplicated cases can be effectively treated surgically, treatment for complex cases remains challenging to surgeons, they wrote. MRI serves as a problem-solving technique for therapeutic planning, preoperative road mapping, and postoperative detection of recurrent or residual disease.
A good understanding of the anatomy and function of the anal sphincter is vital to understand the surgical options for treating fistulous disease, and knowledge of the major anatomical structures is necessary for interpreting and classifying perianal fistulous disease.
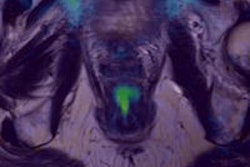
The anal canal lies between the anal verge in the perineum below and the rectum above, the authors continued. The demarcation between the rectum and the anal canal is the anorectal ring/flexure, where the puborectalis muscle forms a sling around the posterior aspect of the anorectal junction.
The internal sphincter is composed of smooth muscle, continuous with the circular smooth muscle of the rectum, and is responsible for 85% of the resting anal tone/involuntary anal continence. It can be surgically divided without causing a loss of continence.
The external sphincter comprises striated skeletal muscle, continuous superiorly with the levator ani muscles. Although responsible for only 15% of the resting anal tone, its strong voluntary contractions resist defecation and are responsible for voluntary continence. A division of the external sphincter can lead to incontinence, they pointed out.
Most perianal fistulas lead to the level of the dentate line, which is also known as the pectinate line. They cannot be seen as a discrete line on MRI, but it is approximately at the midway between the superior border of puborectalis muscle and the inferior border of the external sphincter.
'The anal clock'
"Surgeons describe the site of fistulous tracks by referring to the 'anal clock,' which corresponds to the surgical field-of-view when the patient is placed in the lithotomy position for fistula surgery," the authors wrote. "Therefore, it is helpful to the surgeons if radiologists can use the same surgical reference and describe the MR findings by referring to the anal clock: 12 o'clock = anterior perineum, 3 o'clock = left lateral aspect, 6 o'clock = natal cleft, 9 o'clock = right lateral aspect."
The purposes of classifying perianal fistula are to simplify and standardize communication between clinicians, guide clinicians about the complexity of disease and appropriate treatment options, and advise surgeons with estimates of surgical success and possibility of postsurgical sequelae, especially the dreaded risk of incontinence.
The goal of surgical therapy is the complete eradication of the fistula track while preserving continence, as well as avoiding overly aggressive surgical management and inadvertent sphincteric damage and undertreatment, leading to recurrences or persistence of the fistula, the researchers added. Preservation of fecal continence (i.e., integrity of the external sphincter) is one of the most important considerations during surgical treatment of perianal fistula.
At most institutions, these sequences are used for evaluating perianal fistula:
- T1 and high-resolution T2-weighted sequences without fat saturation for delineation of the muscles, fat planes, and the fistula tract
- T2-weighted sequences with fat suppression for assessing edema and fluid-containing tracts/cavities
- Fat-suppressed T1-weighted pre- and postcontrast-enhanced sequences to assess for the presence of abscesses
When reporting a perianal fistula, the first step is to classify the fistula type. The second step is evaluation of the track content (see table). The track may contain blood products in the immediate postsurgical period, which shows high signal on T1-weighted images, but immediate postoperative MR assessment is rarely performed at Chow's hospital.
| Evaluation of the track content | |||
| Track content | T1 | T2 | Contrast enhancement |
| Filled with granulation tissue | Low | High | + |
| Filled with fluid or pus | Low | High | - |
| Healed track with fibrosis | Low | Low | +/- |
| Seton | Low | Low | - |
Step 3 is identification of associated abscess formation, secondary tracks, and synchronous fistula. Step 4 is identification of the internal opening, and these questions must be addressed:
Why is the internal opening important? Recurrence is almost inevitable if the correct internal opening is not identified and dealt with, as the original source of sepsis will not be eliminated.
Why can't the surgeon "correlate clinically"? Clinical identification of the internal opening can be difficult in some cases. For example, a fistulous track can be difficult to probe if it is narrow, obstructed, kinked, or branched, and forceful probing in such cases will result in the creation of a false track or internal opening.
How can we identify the internal opening? In the axial plane, it is worth remembering the important rule described by David Henry Goodsall in 1900. This rule states that the fistulas with cutaneous openings anterior to the transverse anal line are associated with direct radial fistulous tracks into the anal canal, whereas cutaneous openings posterior to the transverse anal line have tracks that enter the canal in the midline posteriorly. In the coronal plane, the vast majority of the internal openings are located at the dendate line.
How accurate is Goodsall's rule? It is not always accurate, and should be used as a general guide rather than the golden rule in the evaluation of the internal opening, the authors warn.
What if you can't find the internal opening or it is not visible on MRI? "Good luck, but fret not. There are still various ways to examine the internal opening by the surgeon although not with 100% success," they stated.
The co-authors were Drs. Tan Cher Heng, Poh Feng, and Fong Sau Shung.