A fully automated prostate cancer detection system based on multiparametric MRI analysis has shown promise in the detection of high-grade tumors, according to Dutch research. In addition to helping identify cancer locations, a computer-aided detection (CAD) system may help guide biopsy toward the most aggressive parts of tumors.
Systematic prostate transrectal ultrasound (TRUS)-guided biopsy is the standard procedure for prostate histological sampling. However, systematic biopsies do not detect all clinically significant cancers, and efforts are being made to improve the protocols used.
A prostate MRI examination has the potential to improve prostate specific antigen (PSA)-based screening scenarios as a noninvasive detection tool. A number of recent clinical studies have shown that the combination of anatomical, functional, and metabolic MRI information can have a prostate cancer tumor detection accuracy of up to 92% (Physics in Medicine and Biology 2012, Vol. 57:6, pp. 1527-1542).
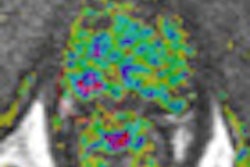
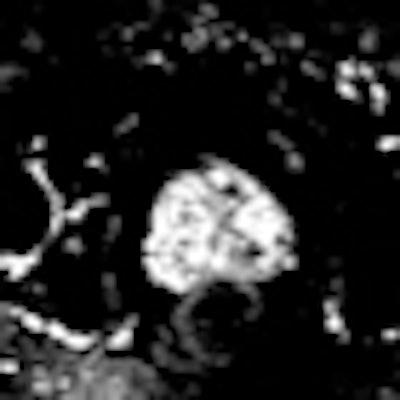
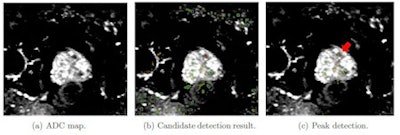 Cross-sectional transversal views of an example apparent diffusion coefficient (ADC) map of a patient with a tumor in the transition zone. (a) Multiple dark blob-like regions are visible in and outside the prostate. (b) The ADC map is shown with the blob likelihood map displayed as a color-coded overlay. Lesion candidates are detected in the pelvis showing false positives outside the prostate. These are ignored using the prostate segmentation. (c) The remaining lesion candidates are displayed within the prostate segmentation. The (red) arrow indicates a tumor with Gleason grade 3+4 which was detected by the peak detector with the highest likelihood of all detected blobs. Image courtesy of Pieter Vos, Radboud University Nijmegen Medical Centre.
Cross-sectional transversal views of an example apparent diffusion coefficient (ADC) map of a patient with a tumor in the transition zone. (a) Multiple dark blob-like regions are visible in and outside the prostate. (b) The ADC map is shown with the blob likelihood map displayed as a color-coded overlay. Lesion candidates are detected in the pelvis showing false positives outside the prostate. These are ignored using the prostate segmentation. (c) The remaining lesion candidates are displayed within the prostate segmentation. The (red) arrow indicates a tumor with Gleason grade 3+4 which was detected by the peak detector with the highest likelihood of all detected blobs. Image courtesy of Pieter Vos, Radboud University Nijmegen Medical Centre."The focus of our research was to detect only high-grade tumors, with the aim of preventing the over-treatment and over-diagnosis of patients that have slow-growing and less aggressive prostate cancers," lead author Dr. Pieter Vos, PhD, told medicalphysicsweb. He developed the CAD technology as part of research undertaken for his doctoral degree at the Radboud University Nijmegen Medical Centre in Nijmegen, the Netherlands.
The technology, for use with multiparametric MRI, demonstrated a sensitivity of 88% and a mean false-positive rate of five findings per patient in patients with aggressive prostate cancer. The efficacy of the CAD system compares well with existing detection methods.
"If you consider that regular ultrasound guided biopsies require at least six tissue cores and detect only 70% of all cancers, our CAD approach is already an improvement. Furthermore, if you consider that the same biopsies under-grades half the aggressive cancers, I would say our approach is fairly good," said senior author Henkjan Huisman, PhD, an assistant professor in the department of radiology and leader of the prostate CAD group at the medical center.
The research is timely, as MRI is under investigation in the Netherlands and in the U.K. as a potential screening tool for prostate cancer. Multiparametric MRI, which demonstrates both anatomy and function, has already shown potential in the detection of prostate tumors. According to Huisman, MRI screening could avoid 50% of biopsies. However, visual analysis of the large data sets by a radiologist is time-consuming and requires a high level of expertise. A high level of interobserver variability has also been reported in clinical studies.
Fully automated approach
The fully automated approach eliminates these limitations, reducing interobserver variability and increasing analysis efficiency. Furthermore, use of the technology has the potential to reduce unnecessary biopsies in patients that have elevated PSA levels, but turn out not to have prostate cancer. The CAD system is also able to pinpoint the most aggressive part of the tumor, and therefore has the potential to guide biopsy site selection and focal therapies such as radiotherapy.
The researchers tested the CAD system with MRI image sets from 200 patients with elevated PSA levels, who had previously undergone an ultrasound guided biopsy that had a negative result. The patients ranged in age from 50 to 69 years, with a mean age of 60. Their mean PSA level was 13.6 ngmL and the mean Gleason score was 7.3. Three weeks after a transrectal-ultrasonographically-guided sextant biopsy of the prostate had been performed, each patient had multiparametric imaging using a 3.0-tesla whole-body MR scanner (Trio Tim, Siemens Healthcare) that included a T2-weighted volume and a contrast enhanced 3D T1-weighted scan.
Perfusion maps were generated from the contrast enhanced images. Apparent diffusion coefficient (ADC) maps were derived using diffusion weighted imaging. Visual analysis of the images by a radiologist and MRI guided biopsy provided a reference standard with which to assess CAD accuracy.
Three-step lesion detection
The CAD system identifies suspicious prostate lesions using three key steps. Firstly, voxel classification, using a blob detection algorithm, is applied to the ADC map. The algorithm identifies dark regions within the entire imaged volume that may or may not represent malignant tissue. Secondly, automated segmentation is used to define the prostate outline, which in turn is used to limit the search for lesion candidates to within the gland. Thirdly, the suspicious locations remaining after segmentation are analyzed using a histogram-based approach and a set of objective criteria, in order to identify malignant tissue.
In addition to the 88% sensitivity reported in the detection of high-grade tumors, the researchers also detected 74% of all tumors, with an average of five false-positive sites per patient.
The group is now investigating refinements to the prostate CAD system and is applying the same approach to MRI lymphography, also for use in prostate cancer patients. In parallel, they are working on technology that will use the CAD system output to guide ultrasound guided biopsies, using dedicated image registration techniques.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.