Noncontact ultrasound imaging, in which the transducer is separated from the skin by air, has been achieved in vivo by researchers. The group is cautiously optimistic about a clinical future for the technique, which uses a tightly focused high-intensity beam to generate tomographic images.
"The project is definitely in its infancy, but the results to date have been very encouraging," said Gregory Clement, PhD, physicist and first author of the study conducted at the University of Electro-Communications in Tokyo (Physics in Medicine and Biology, 21 September 2013, Vol. 58:18, pp. 6263-6278).
Without good contact between the transducer and the skin using acoustic coupling gel, the beam used in conventional ultrasound encounters a large acoustic impedance mismatch between the transducer and the air in front of it that prevents transmission. This limits the use of ultrasound in some clinical scenarios, including patients with open wounds and where sterile conditions are required, such as in surgery.
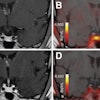
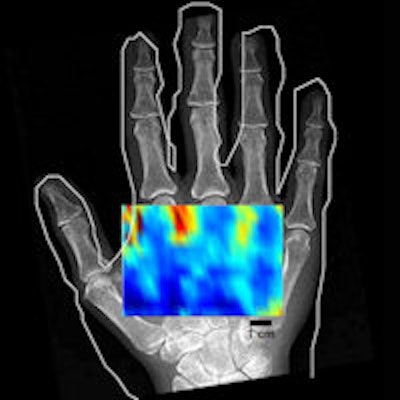
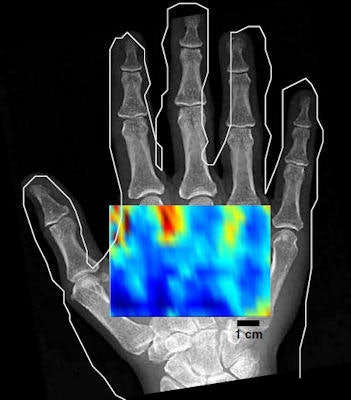 An in vivo low-resolution C-mode noncontact image of a hand shows varying contrast between the anatomy containing mainly bone and that containing only soft tissue.
An in vivo low-resolution C-mode noncontact image of a hand shows varying contrast between the anatomy containing mainly bone and that containing only soft tissue.To overcome this, Clement and his collaborators investigated whether the greater focusing potential of ultrasound in air, in which focal diameters one quarter of that possible in tissue can be achieved, could be exploited to enable noncontact imaging. High-beam intensity in air compensates for the low transmission of the beam across the air-skin boundary.
A virtual transducer
The group's approach uses a bowl-shaped transducer to focus an ultrasound beam into a 5-mm spot at the skin surface. The spot generates a point source of ultrasound that, when scanned over the surface of an object, can be used to perform diffraction tomography.
"The method treats the skin surface as a 'virtual' transducer, allowing for a large effective number of sources and receivers, thus opening the potential for large regions to be imaged," said Clement, who now works at the Cleveland Clinic in Ohio in the U.S. "Current medical probes can't conform to the body, thereby limiting where they can be placed," he added.
A 40-kHz transducer was simulated and constructed for the preliminary testing of the imaging technique. Though a low, suboptimal frequency for imaging, elements capable of emitting 40 kHz are commercially available at low costs and the researcher's goal was to provide proof of principle, rather than design a clinical specification imaging system.
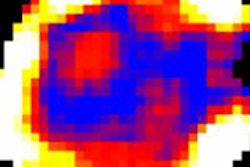
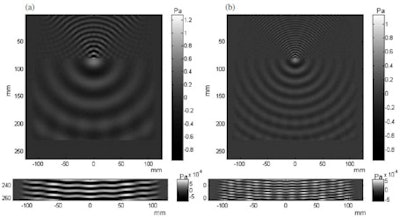 Simulation of a 40-kHz beam (left) and the first harmonic at 80 kHz (right) show the generation of a point ultrasound source and spherical wavefronts at an air-water interface.
Simulation of a 40-kHz beam (left) and the first harmonic at 80 kHz (right) show the generation of a point ultrasound source and spherical wavefronts at an air-water interface.Simulations predict feasibility
The researchers used simulations to demonstrate the feasibility of the technique, predicting a measurable exiting signal from the skin of around 1 mPa from an incident focal pressure of 162 dB (2.5 kPa).
An optimum transducer geometry with a 175-mm diameter and 90-mm radius of curvature capable of producing a 5-mm-wide focal spot and a peak pressure of 3.2 kPa was also predicted. This guided the construction of a transducer prototype with 400 elements arranged in a hemispherical array, which demonstrated the physical feasibility of the approach.
After beam characterization and transmission measurements, images of a phantom and a hand were acquired in vivo using the transducer and a broadband microphone receiver. An image of three 3-mm wooden rods in a water phantom, scanned axially, demonstrated the tomographic reconstruction approach, albeit with some image distortion and artifacts. In vivo noncontact imaging of a hand was demonstrated with a conventional C-mode approach that produces images for a fixed depth below the skin. The low-resolution scan shows varying contrast between the anatomy containing mainly bone and that containing only soft tissue.
Clement noted that the group will continue the development and clinical testing of the noncontact imaging technique over the next few years. Ongoing work in the lab includes receiver optimization to increase detected signal strengths and therefore technique sensitivity and the investigation of faster acquisition techniques to reduce scan times; the point-by-point acquisition method used in the hand scan took 10 hours.
The team is also developing a new reconstruction algorithm, as an assumption of existing diffraction tomography reconstruction approaches of a slowly varying skin curvature cannot be met in clinical imaging.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.