Low-dose CT has proved to be pivotal in the early detection of lung cancer in a groundbreaking U.K. lung cancer screening pilot project that aimed to discover if CT was a viable cost-effective option. The findings were published online by BMJ on 8 December.
In a randomized controlled trial involving people at high risk of lung cancer as selected by the Liverpool Lung Project (LLP) validated risk prediction model, researchers found a single low-dose CT (LDCT) scan led to a 2.1% detection rate with 86% stage I and II and an 83% resection rate.
The U.K. Lung Cancer Screening (UKLS) pilot trial is thought to be the first to use a true population approach to selection with a validated individual risk assessment, and shows that, with volumetric nodule measurement and prespecified clinical pathways, it is possible to detect lung cancer at an early stage and deliver potentially curative treatment in more than 80% of cases. Data on observed lung cancer mortality reduction may confirm initial health economic analysis that suggests intervention would be cost-effective.
In the U.K., around three-quarters of patients present with advanced lung cancer when treatment has little effect on survival, according to lead author John K. Field, PhD, professor of molecular oncology (clinical) at the University of Liverpool. The UKLS pilot showed that screening can detect cancers early. Key findings included 34 cancers discovered at baseline in 1994 patients screened (1.7% lung cancer prevalence), with eight (0.4%) at the 12-month scan. Furthermore, 28 out of the 42 confirmed cancers (66.7%) were at stage I and considered to have a good survival outcome prediction. Results are summarized in the table below.
| Number of participants screened with LDCT | 1,994 |
| Number of confirmed cancers overall | 42/1,994 (2.1%) |
| Number of cancers found at baseline scan | 34/1,994 (1.7%) |
| Number of cancers found at 12 month scan on individuals with category 2 or 3 nodules discovered in baseline scan | 8/951 |
| Stage I lung cancer | 28/42 (66.7%) |
| Stage I or II lung cancer | 36/42 (85.7%) |
| Surgical resection | 35/42 (83.3%) |
| Subjects with nodules greater than 5 mm3/5 mm diameter | 536 |
| Of these, subjects found to have lung cancer | 42/536 (including 1 in follow-up of nodules between 15 and 50 mm3 at 12 months) |
| Baseline estimate for the incremental cost-effectiveness ratio of once-only CT screening in the pilot UKLS | 8,466 pounds (11,651 euros) per quality adjusted life year gained |
The LLP Risk Questionnaires about lifestyle and history were sent to 247,354 individuals ages 50-75 across six healthcare areas, to identify those at high risk (≥ 5% over five years) of developing lung cancer. Of those 247,354 who were approached, 8,729 (11.5%) were eligible and 4,055 were randomized into a CT screen arm or a no screen arm at the Liverpool Heart & Chest Hospital National Health Service (NHS) Foundation Trust, Liverpool, and the Papworth Hospital NHS Foundation Trust, Cambridge.
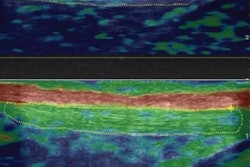
Of these 4,055 randomized participants, 2,028 went into the LDCT arm (1,994 underwent LDCT), while the rest underwent no screening. The CT images of the screened patients were subject to a first and second read by two experienced thoracic radiologists, using volumetric analysis. Second reads of all the CT scans were undertaken at the Royal Brompton and Harefield NHS Foundation Trust.
Depending on the category of the nodule found, recruits were streamed into a UKLS care pathway, category 1, no further action, category 2, repeat scan at three months and if positive, scan again at nine months, category 3, repeat scan at 12 months or category 4, refer to multidisciplinary team for clinical workup and treatment. Scans were performed on 64-slice and 128-slice scanners.
Forty-two of the 1,994 screened participants (2.1%) had confirmed lung cancer, 34 (1.7%) at baseline and eight (0.4%) at the 12-month scan. Of 42 confirmed cancers, 28 (66.7%) had stage I disease, 36/42 (85.7%) had stage I or II disease, and 35/42 (83.3%) had surgical resection. Five hundred and thirty-six subjects had nodules greater than 50 mm3 or 5 mm diameter, and 41/536 were found to have lung cancer.
 The results of the UKLS trial will affect the decision to run a national lung cancer screening program in the U.K., according to John K. Field, PhD.
The results of the UKLS trial will affect the decision to run a national lung cancer screening program in the U.K., according to John K. Field, PhD.One further cancer was detected by follow-up of nodules between 15 mm3 and 50 mm3 at 12 months. The baseline estimate for the incremental cost-effectiveness ratio of once-only CT screening, under the UKLS protocol, was 8,466 pounds (around 11,600 euros) per quality-adjusted life year gained (confidence interval 5,542 pounds to 12,569 pounds, or 7,600 to 17,300 euros).
"This was the first U.K. lung cancer randomized CT screening trial ... demonstrating that we have a validated method in place to select and recruit individuals with a high risk of developing lung cancer, utilizing the risk prediction model LLPv2, plus a cut-off of 5% and above risk over five years," Field told AuntMinnieEurope.com. "The specific successes of the UKLS trial include the demonstration that a population-based lung cancer screening trial can be undertaken in the U.K., using a risk-based prediction model to select participants. The UKLS protocol-driven radiology, with volumetric analysis, and the UKLS care pathways have ensured the highest level of CT assessment and management of participants, as they progressed through the trial."
Field, who is director of research at the Roy Castle Lung Cancer Research Program in Liverpool and visiting professor at University College London, underlined the most significant clinical finding being the 1.7% prevalence of lung cancer at baseline, and the finding that 66.7% were stage 1, and considered to have a good five year clinical outcome.
"Almost half of the subjects with confirmed lung cancer were in the most deprived socioeconomic quintile. The baseline prevalence rate is considerably higher than that reported by the U.S. National Lung Cancer Screening Trial (NLST) or [the Netherlands'] NELSON trial," he added. "Over 80% were early stage disease (stage I and II); and over 80% had surgical resections -- which is much higher than the average surgical resection rate in the U.K. in non-small cell lung cancer (NSCLC) of 20%."
75% late stage
Almost three-quarters of people in the U.K. with lung cancer present with advanced stage disease when treatment has little effect on survival, according to Field et al. They point to the NLST, which was stopped a year early in 2010 because a 20% relative reduction in lung cancer mortality had been achieved by LDCT compared with chest x-ray after three annual screens and six years of follow-up.
However, during the first International Association for the Study of Lung Cancer (IASLC) CT screening Workshop in 2011, at which Field was a moderator, areas of improvement were recommended pertaining to identification of high-risk individuals, radiology guidelines, guidelines for pathology reports, and clinical workup of indeterminate nodules, plus definition of criteria for surgical and therapeutic interventions of suspicious nodules identified through lung cancer CT screening programs, and a method to encourage recruits to stop smoking during screening programs.
Clever pilot design
In line with all these IASLC recommendations, the pilot UKLS aimed to demonstrate the effectiveness of risk prediction modeling for the selection of high-risk participants, to evaluate the use of volumetric analysis in the management of CT-detected nodules linked with pragmatic follow-up strategies, and to determine cost-effectiveness based on modeling of the pilot UKLS approach with reference to NLST mortality reduction. The surgical team for referred recruits also worked on therapy criteria, while the screening arm involved lung function and lung age demonstrations of screened subjects as part of a "stop smoking" strategy.
Modeling the cost-effectiveness, based on the UKLS baseline CT scans, demonstrated that CT screening could potentially be cost-effective in the U.K.
"The results of this trial will contribute to the decision to run a national lung cancer screening program in the U.K., however, as this was a pilot, we need to await the results of the large Dutch trial for mortality data. The plan is to pool the UKLS data with the NELSON trial data," he stated.
Tailored radiological approach
The UKLS trial incorporated nodule volumetric software as part of its protocol; this provides a more accurate and reliable measurement of lung nodule size and growth than diameter measurements, according to Field. Despite this, however, a major implication of the findings from the UKLS trial is the need to lessen the burden of diagnostic workup of indeterminate nodules and the potential of deploying trained radiographers to contribute to any future screening program under the supervision of a consultant radiologist. This, Field believes, was successfully tested within the UKLS trial, the full article about which can be accessed here.
He pointed to the success of NLST, in which more than 50,000 people showed a 20% mortality advantage in the CT screen arm, and based on this, the U.S. Preventive Services Task Force (USPSTF) recommendation was to introduce screening in the country, which is now funded by Medicare.
Meanwhile, in Liverpool, the Liverpool Clinical Commissioning Group is organizing the Liverpool Healthy Lung Project, which is aimed at identifying high-risk people and will also provide advice on smoking cessation. The details of this program will be launched next year.
"The bottom line is if we could detect lung cancer at an earlier stage through a CT screening program it would have a major impact on the diagnosis and improve the survival rates of this devastating disease," he said.