Diffusion-weighted MRI (DWI) is similar to -- and probably a little better than -- conventional black blood short tau inversion-recovery (STIR) MR images when it comes to detecting edema in patients with myocarditis, the authors of a new study from Spain have found.
Rather than the standard black blood STIR protocol, the researchers pioneered a high b value DWI protocol to detect edema in patients with acute myocarditis.
They found no significant differences in the results between STIR and DWI, but slightly higher sensitivities and positive predictive values for the latter. And the effects of edema on the myocardium were much more conspicuous on the DWI protocol, earning the new technique slightly better results overall.
MRI is an important modality for detecting acute myocarditis, which is turning out to be a bigger clinical problem than foreseen just a few years ago, said Dr. Jordi Broncano in a talk at ECR 2014 in Vienna.
 Dr. Jordi Broncano from Hospital Cruz Roja and Hospital San Juan de Dios in Córdoba, Spain.
Dr. Jordi Broncano from Hospital Cruz Roja and Hospital San Juan de Dios in Córdoba, Spain.Established MR criteria for diagnosing acute myocarditis include increasing T2 signal in the myocardium, indicating edema; increased global myocardial enhancement suggesting hyperemia or capillary fluids; and focal late gadolinium enhancement with nonischemic distribution, suggesting fibrosis or necrosis of the myocardium.
"The presence of at least two of these factors is necessary to make a diagnosis of acute myocarditis," said Broncano, from Hospital Cruz Roja and Hospital San Juan de Dios in Córdoba, Spain.
Can DWI do the job better? DWI is known to increase signal intensity in the myocardium compared with black blood STIR images. But there are only three reports of DWI for that purpose in the literature, with studies using a variety of imaging parameters, but all using low b values.
What are they? All DWI scans are characterized by their b values (measured in s/mm2), which are a function of diffusion gradient strength, duration of the gradient, and the interval between the different diffusion gradients. Potet et al reported optimal detection of myocardial viability at 300 s/mm2, he said.
One study was published by Potet and colleagues (Radiology, November 2013, Vol. 269:2, pp. 362-369) using single-slice, four-chamber-oriented low b value (50 s/mm2) DWI with cardiac gating and respiratory synchronization, Broncano told AuntMinnieEurope.com.
"That's why we tried to evaluate a whole cardiac and high b value, attending to the evaluation of the myocardium, for the detection of edema in patients with acute myocarditis," he noted in an email.
In their study, Broncano et al examined the DWI detection capability of myocardial edema in patients with acute myocarditis, comparing it with black-blood STIR and its accuracy in combination with delayed gadolinium enhancement for the diagnosis of acute myocarditis.
 Acute myocarditis seen at (clockwise from upper left), low b value MRI, high b value MRI, short-tau inversion recovery (STIR), and late gadolinium enhancement (LE). All images courtesy of Dr. Jordi Broncano.
Acute myocarditis seen at (clockwise from upper left), low b value MRI, high b value MRI, short-tau inversion recovery (STIR), and late gadolinium enhancement (LE). All images courtesy of Dr. Jordi Broncano.Black blood STIR images deliver moderate sensitivity for edema in the setting of acute myocarditis: 45% to 100% sensitivity, 50% to 100% specificity, 59% to 79% accuracy overall, he said. The aim was to assess the clinical feasibility of whole cardiac high b value DWI of myocardial edema in acute myocarditis compared with standard [cardiac MR] techniques, Broncano said.
The study began with 117 patients presenting with clinically suspected myocarditis between 2009 and 2014. After applying exclusion criteria they ended up with 29 patients (mean age 38.54 ± 15.71 years) including eight women and 21 men with clinically confirmed acute myocarditis, who were scanned on a 3-tesla MRI scanner (n = 11) and a 1.5-tesla scanner (n = 18). The mean delay time from symptom onset to MR was about eight days.
The group performed both short-axis black blood STIR images and late-enhancement 3D inversion recovery T1 sequences. Late gadolinium enhancement combined with clinical information served as the reference standard due to its high specificity and good sensitivity for detecting acute myocarditis, Broncano said.
DWI imaging consisted of a single-shot spin-echo breath-hold DWI sequence applied with prospective ECG triggering in diastole, and selective fat-suppression techniques were also applied.
The data were read by two experienced readers who interpreted the images in two separate sessions: first the short-axis black blood STIR, and second DWI with late gadolinium enhancement.
They documented the presence of myocardial edema in black blood STIR and DWI images and its effect on the myocardium, as well as late gadolinium enhancement, its extent, affect on the lateral wall, and topography determined by calculating the T2 ration between the myocardium and skeletal muscle.
Similar, with a slight edge for DWI
"Both STIR and DWI with late gadolinium enhancement showed high sensitivity and positive predictive value for both readers, with excellent interobserver agreement," Broncano said. "No significant variations were observed in the extent of myocardial edema between the STIR and DWI, although the conspicuity of affected myocardium was greater on the DWI."
','dvPres', 'clsTopBtn', 'true' );" >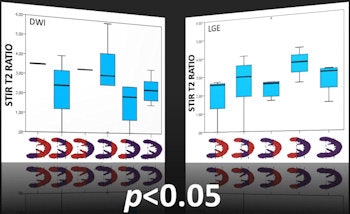
The results also showed significant differences in the extension of affected myocardium between the STIR and DWI protocols (p = 0.013), but no significant differences in lateral wall extension (p = 0.371) or topography (p = 0.040) between the two techniques.
Minor artifacts and distortion were present on isolated slices -- and more frequent on 3-tesla images -- but did not prevent the adequate evaluation of myocardial edema, Broncano said.
"High b value breath-hold DWI is similar to black blood STIR images for detection of myocardial edema in the setting of acute myocarditis, with excellent interobserver agreement," he concluded. So if the results are similar, why is DWI potentially better?
"Because in the same patients we have observed that the conspicuity of edematous regions is higher that on STIR images," Broncano told AuntMinnieEurope.com, noting that the results are still preliminary.
The next step will be a semiquantitative analysis comparing STIR and DWI in patients with acute myocarditis and healthy control subjects in order to establish effective threshold values and data on sensitivity, specificity, positive predictive value, and negative predictive value.
"Also, evaluation of the behavior of myocardial edema in low and high b value comparatively and the follow-up behavior will be really interesting in order to identify those patients that will have better outcomes," he wrote.
The latest results have been submitted to RSNA 2014 including a semiquantitative analysis of DWI and including healthy control subjects.