In stroke treatment, time is brain, as they say, but the timely detection of acute intracranial hemorrhage (AIH) can be difficult when dealing with subcentimeter lesions or inexperienced readers. A new computer-aided detection (CAD) system designed to detect blood clots in the brain could be a welcome addition.
"The presentation [of AIH] can be caused by a stroke or by a head injury, and it's very important to find these hemorrhage patients," said T. Chan, PhD, from Hong Kong Polytechnic University. AIH is defined as bleeding in the skull occurring within the previous 72 hours. Different patients require different treatment strategies, Chan said in a presentation on CAD software developed at the university at the 2010 Computer Assisted Radiology and Surgery (CARS) meeting in Geneva.
Working in the CT-based CAD system's favor are the wide natural attenuation differences between blood and clots and brain. A combination of high protein content and low water means that "blood clots actually have high density compared to blood and parenchyma, which makes the clots readily distinguishable on an automated system using CT images," he said. "From our measurements, the acute blood clot, depending on the blood thickness, ranges from 40 to 100 HU. Brain parenchyma is 35 to 60 HU, so there's kind of an overlap."
Yet CAD is needed because AIH isn't always obvious. "Physicians aren't perfect -- only about 78% accurate -- so we designed a system to help make that decision with them," Chan said.
The investigational CAD scheme was trained using 5-mm and 10-mm CT slices, and it's executed on a slice-by-slice basis, he explained. The CAD scheme is aimed at improving the accuracy of AIH management and decreasing the risk of misdiagnosis and mismanagement. It is designed for use by clinicians other than radiologists -- who tend to do a pretty good job of finding the high-attenuating blood clots on their own, Chan said.
The processing begins with CAD segmentation of the intracranial contents using thresholding and morphological operations, followed by denoising and adjustments for CT cupping artifacts. Once the brain is realigned into a normal position, AIH candidates are selected based on top-hat transformation and left-right asymmetry. Finally, the results are adjusted using a normalized coordinate system, Chan said.
"We acquire CT of the brain and we extract hematomas by using a global comparison between both sides of the brain," Chan said. Anatomy helps the CAD algorithm significantly in detecting irregularly shaped regions of bleeding.
"Because AIH comes in all kinds of sizes and shapes, we find that many different image features do not work simply because it's so varied. But we found that there are certain features depending on which part is the blood or parenchyma," Chan said. "For example, blood occurring in the peripheral region will be limited by the bone outside and the brain inside. That means it will conform to a certain shape that is basically limited by the anatomic region. For blood within the brain, parenchyma [clots] tend to be more round."
Testing 1, 2, 3
The investigators performed several experiments using the algorithm, the first of which validated the CAD scheme on 22 positive cases and 44 controls. It generated a sensitivity of 83% on a per-lesion basis, and a false-positive rate of only 0.29 per case or 0.02 per image, Chan said.
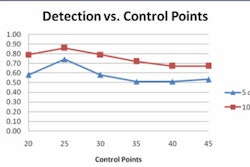
Next, a receiver operator characteristics (ROC) curve study was performed by emergency physicians and radiology residents using the CAD system on 30 studies with AIH smaller than 10 mm, as well as 30 controls.
According to these results, the average ROC(AZ) increased from 0.8422 to 0.9244 (p = 0.0107) for the ED physicians and from 0.9371 to 0.9762 (p = 0.0088) for the radiology residents with use of the CAD.
Cases in which physicians changed diagnostic decisions post-CAD
|
||||||||||||||||||||
| The proportion of correct changes relative to incorrect changes increased from emergency physicians to radiology residents to radiology specialists. The total and relative numbers of changes decreased from emergency physicians to radiology residents to radiology specialists. |
"Emergency physicians not sure of the findings changed their minds a lot" when confronted with CAD results, Chan said. "Most of the changes were because they had missed something in the first place, but it was also encouraging to see that they are swayed by the accuracy of the CAD. The radiology residents also changed their minds a lot, but they were less swayed by the incorrect results of the CAD."
On the other hand, the radiology specialists weren't helped significantly by CAD, and they only rarely changed their minds after seeing a CAD result contrary to their initial decision, Chan said.
In a final, standalone test for the CAD system, 138 patients from Los Angeles County + University of Southern California (LAC+USC) hospital reported to have AIH underwent image analysis using CAD, and they were matched by age, sex, and ethnicity with control patients. In this test, the reported sensitivity of the system was 69.6%, Chan said. Out of 104 true-positive cases, the system generated 31 false negatives, confirming that the "algorithm needs improvement," he said.
The research continues, Chan said, and a more advanced 3D version of the software is expected to improve sensitivity by eliminating the artifacts associated with 2D image reconstructions.
"The early results are encouraging, with good sensitivity and a very low false-positive rate," he said. "We hope it can help with reading."
By Eric Barnes
AuntMinnie.com staff writer
September 20, 2010
Related Reading
Gold in scan finds dangerous artery clogs: U.S. study, August 18, 2010
Internal anomalies common in children with large facial hemangiomas, July 22, 2010
Study offers strategy for managing incidental findings on fMRI, July 6, 2010
Incidental findings are common on brain MRI: meta-analysis, August 26, 2009
Incidental findings on brain MRI common as technology advances, November 1, 2007
Copyright © 2010 AuntMinnie.com