The British have "highly variable views" about how much overdetection they would accept in cancer screening, according to a study published online March 3 in BMJ.
Overdetection occurs when cancerous lesions are found and treated, but would not cause symptoms or become fatal during a person's lifetime. Researchers from the University of Oxford Nuffield Department of Primary Care Health Sciences said screening "should include clear information on the likelihood and consequences of overdetection to allow people to make an informed choice."
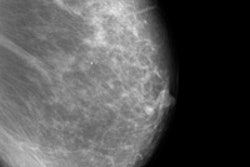
The findings come from an online survey of 1,000 people in the U.K. who were at least 18 years old. The composition of participants was representative for age and sex according to the 2011 U.K. census. The survey included questions about breast cancer screening for women, prostate cancer screening for men, and bowel cancer screening for both sexes. For each type of cancer screening, researchers showed the number of cases per year in the U.K. and a description of the treatment, including adverse effects.
They then presented two different screening scenarios. One case indicated a 10% reduction in cancer-specific deaths, and the second proposal indicated a 50% reduction. Respondents were asked the maximum number of people overdetected and overtreated that they would accept for the given benefit.
Up to 7% said they would accept no overdetection at all, compared with 14% who would accept overdetection in the entire population. Across the different cancer types, people would accept a median of 113 to 150 people (per 1,000 cases) to be overdetected to avoid one person dying of cancer as a result of screening.
People also accepted more overdetection when they perceived a higher benefit from cancer screening from a 10% mortality reduction to 50% mortality reduction.
The study showed that acceptability of overdetection for bowel cancer screening was significantly lower than for breast cancer screening in women and prostate cancer screening in men.
Generally, people 50 years old or older accepted less overdetection, compared with people with a higher education who accepted more. People with a chronic condition also were more likely to accept overdetection in at least 80% of the screened population.
In a related commentary in BMJ, Alexandra Barratt, MBBS, MPH, PhD, a professor of public health at the University of Sydney School of Public Health, argued that clinicians should think twice before introducing new breast imaging technologies, such as tomosynthesis or extending screening to older and younger women, until incremental net benefit to women has been demonstrated in high-quality studies.
In 2012, an independent U.K. panel estimated that about 19% of breast cancers diagnosed among women invited to mammogram screening were in fact overdia