Radiologists spend significantly more time observing mediolateral oblique (MLO) breast images and right images, according to Irish research using eye-tracking software. This knowledge may be useful to help remove any interpretation differences and as a feedback tool.
It's early days for perception studies, but they're important because an understanding of a radiologist's eye movements can shed light on interpretation behavior, noted Wijdan Alomaim, a doctoral candidate for breast imaging at University College Dublin, in an interview with AuntMinnieEurope.com.
"Eye tracking is still a new subject, but it's often used for pathology," she said, adding that mammography is more complicated because it involves multiple images.
Studying behavior and fixation time
Fixation time has been found to be associated with true- and false-positive decisions, so the longer the fixation time, the more false-negative decisions will be made, Alomaim noted.
"Scanning a certain side of the breast for a longer time raises the question if this behavior is one of the many reasons for missing cancers," she said.
In a study presented at last month's ECR 2016, the Dublin team sought to determine not only radiologists' behavior when interpreting mammographic images, but also whether breast density plays a role in fixation time. Breast radiologists from the U.K. were voluntarily recruited to review sets of anonymized mammographic images (n = 170) and to subjectively rate the breast density according to the BI-RADS categorization.
A Tobii eye tracker was used to observe the eye movement of the radiologists while assessing the images. The eye tracker uses a 23-inch monitor with a screen resolution of 1,920 x 1,080 pixels attached to eye-tracking equipment with a high-speed infrared camera that also releases infrared light. It can track data on eye pupil movement at 60 Hz, 120 Hz, or 300 Hz with high accuracy and provides solid eye tracking for large head movements while assessing the images on the screen.
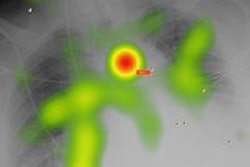
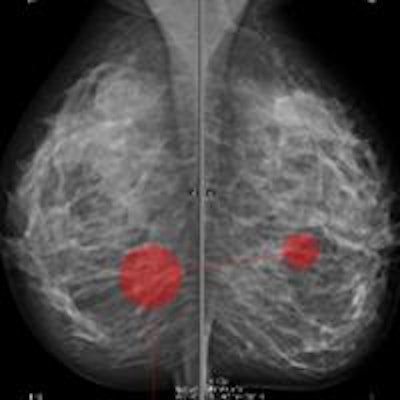
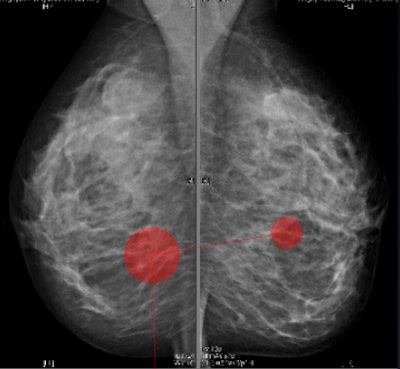 Screenshots of the Tobii eye-tracking software. The radiologists' eye fixations are the red dots. The size of the dot represents the fixation duration time: the bigger the dot, the longer the fixation time. Images courtesy of Wijdan Alomaim.
Screenshots of the Tobii eye-tracking software. The radiologists' eye fixations are the red dots. The size of the dot represents the fixation duration time: the bigger the dot, the longer the fixation time. Images courtesy of Wijdan Alomaim.The researchers obtained data obtained for 17 radiologists, who reviewed the mammography images using standardized viewing conditions and Ziltron software. Results showed the radiologists spent significantly more time observing MLO (MLO: 1.67 sec. versus CC: 1.32 sec.) and right images (right: 1.63 sec. versus left: 1.36 sec.). They also spend significantly more time observing images with BI-RAD 3 (mean = 1.48 sec.) density than the other BI-RADS categories.
Improving training
"The impact of breast density on radiologist fixation time in mammography varies according to the density," Alomaim noted during her talk at ECR 2016. "The variation in how radiologists viewed projections and different sides of the breast warrants further research, as does potential impact upon abnormality identification. An understanding of radiology review patterns will inform training and support the amelioration of potential interpretation differences."
For instance, knowing radiologists favor a certain side of the breast will draw attention to this, which can be passed on to a trainee and thus avoided, she explained.
Since ECR, Alomaim is planning -- due to the positive, initial research findings -- to extend the work to a different environment, such as recording the searching pattern and the fixation time for radiologists on their daily reporting working routine.
"Also, these findings can lead to a lot of other future research ideas that could help in reducing the interreader variability between the radiologists, as well as increasing the breast cancer detection," she explained.