The combination of standard PET/CT with respiratory-gated PET/CT can significantly improve the diagnosis of small colorectal liver metastases, but patient cooperation is a must for a successful scan, according to a Norwegian study published online on 14 May in the European Journal of Radiology.
Researchers from Oslo University Hospital found that the few additional minutes it takes to perform a respiratory-gated PET/CT scan can increase sensitivity. But the key factor to successful scans is a patient's ability to maintain the same position during that additional time to ensure correct registration and attenuation correction between PET and CT images.
Lead author Dr. Anselm Schulz, from the hospital's department of radiology and nuclear medicine, and colleagues conceded that it is a "major challenge" for many patients to perform breath-holds during respiratory-gated PET acquisitions, but the benefits of the imaging technique could be accomplished by restricting patient motion.
PET/CT limitations
According to one meta-analysis, MRI generally is accepted as the best modality to diagnose colorectal liver metastases, but FDG-PET/CT can achieve comparable sensitivity. The 2010 study also suggested FDG-PET and FDG-PET/CT may be "second-line" options when MRI is unable to characterize liver lesions (Radiology, December 2010, Vol. 257:3, pp. 674-684).
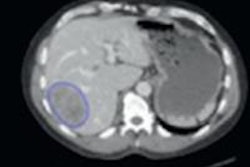
Lower spatial resolution, high normal liver FDG uptake, and reduced conspicuity of focal FDG uptake due to respiratory motion can hinder PET/CT's diagnostic performance compared with MRI, Schulz and colleagues noted. The discrepancy in performance is particularly apparent with metastatic lesions smaller than 10 mm in size. Therefore, the objective of team's study was to determine if adding a breath-hold, or respiratory gating, approach has any diagnostic value when scanning patients with suspected colorectal liver metastases.
Their prospective study included 43 patients who were scheduled for resection for suspected colorectal liver metastases between September 2011 and January 2013. All 26 males and 17 females (mean age of 65.7 ± 10.5 years) received PET/CT and respiratory-gated PET/CT during the same imaging session, but none of them had yet received treatment for their metastases.
Standard PET/CT (Biograph mCT, Siemens Healthcare) was performed with time-of-flight imaging after patients fasted for at least six hours. The scan covered an area from skull base to proximal thighs 60 minutes (± 10 minutes) after intravenous administration of FDG (based on a patient's body weight) with an acquisition time of two minutes per bed position.
Immediately after the standard PET/CT scan, patients were asked to remain still for another six minutes to complete a respiratory-gated PET/CT scan of the liver.
To help patients with their breathing patterns, researchers used a device that displays a color-coded countdown from 9 to 0. Patients were told to hold their breath in moderately deep inspiration during the nine-point countdown, then were allowed to breathe freely for another count of nine. The data derived from the breath-hold period was used to reconstruct respiratory-gated sequences.
Imaging evaluation
Two readers evaluated the results and reported on the number of metastases, their size, and locations. They also rated diagnostic confidence for colorectal liver metastases based on a four-point scale, with 1 as "probably not present" to 4 as "definitely present." Only lesions assigned with a score of 3 or 4 were considered colorectal liver metastases.
The interobserver agreement for PET/CT and respiratory-gated PET/CT was almost identical, with kappa values of 0.86 and 0.83, respectively, for colorectal liver metastases.
Using the reference standard of histopathological confirmation, 311 liver lesions were discovered, with 131 (42%) of those lesions identified as colorectal liver metastases in 39 of 43 patients. Additionally, histopathology confirmed 73 (56%) of 131 colorectal liver metastases.
In a comparison of the hybrid modalities, PET/CT alone and respiratory-gated PET/CT alone achieved relatively similar sensitivity, but the combination of PET/CT and respiratory-gated PET/CT overall was significantly more sensitive than either modality independently for colorectal liver metastases.
| Per-lesion detection of colorectal liver metastases | ||
| Modality | Sensitivity | Positive predictive value |
| PET/CT | 60.0% | 97.5% |
| Respiratory-gated PET/CT | 63.1% | 95.3% |
| Standard PET/CT & respiratory-gated PET/CT | 67.7% | 93.6% |
"Our results showed no significant differences in sensitivity between PET/CT and respiratory-gated PET/CT, although a tendency toward improved sensitivity for respiratory-gated PET/CT was found," the author wrote. "That tendency was expressed by a larger number of additionally identified colorectal liver metastases by respiratory-gated PET/CT, which were not identified by PET/CT. Most pronounced was the difference for colorectal lesion metastases of less than 10 mm."
Noisier images?
The study authors also noted that standard PET/CT produced false-positive results for two lesions, compared with four false-positive lesions with respiratory-gated PET/CT.
Researchers also evaluated the standard deviation of standardized uptake values (SUVSD) to create a quantitative measurement of image noise, which can adversely affect image quality and make colorectal liver metastases more difficult to detect. Standard PET/CT registered an SUVSD of 0.29 (± 0.08), which was significantly less than 0.36 (± 0.08) for respiratory-gated PET/CT.
"Patient-dependent factors were probably the main reason for the limited diagnostic performance of the respiratory-gated PET/CT and the overall higher noise level of the respiratory-gated PET/CT, indicated by significantly increased SUVSD values," Schulz and colleagues stated.
The issue, researchers noted, is patients' inability to maintain the same position during the additional six minutes of respiratory-gated image acquisition time might have affected image results.
"It remains a major challenge that many patients perform a deep inspiration during the CT and then gradually decrease the amplitude of the inspiration during the respiratory-gated PET acquisition," they wrote. "That causes misregistration between PET and CT and imprecise attenuation correction. A possible solution to overcome that issue might be the use of an adjustable mechanical bracket to restrain the inspiratory motion of the thorax at a fixed position."