Researchers from one of Europe's top cancer research facilities think they have achieved a technological milestone by successfully developing a patient-specific molecular imaging phantom using a 3D printer, according to a study published in the August issue of Medical Physics.
Researchers from the Royal Marsden National Health Service (NHS) Foundation Trust and Institute of Cancer Research in Sutton, U.K., are optimistic the phantom can be easily reproduced and future advances in technology will allow for inexpensive manufacture of the devices using this method. Perhaps the most advantageous finding is that the phantom was designed using standard nuclear medicine processing software, which is available from the Internet.
The phantom's final print material was made of clear, solid acrylic plastic, which the authors described as "watertight and rigid" and able to "withstand multiple assembly and scanning protocols," wrote lead author Jonathan Gear, PhD, a clinical scientist at the Royal Marsden's joint department of physics (Med Phys., August 2014, Vol. 41:8).
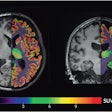
The study also concludes that organ geometry showed good correspondence with anatomical references and the methodology can be applied to other anatomical or geometrical phantoms for molecular imaging.
Costly phantoms
Anatomical phantoms are used regularly in molecular imaging to assess image quality, but, as the authors noted, the devices are often expensive and are not designed for a specific patient population or cohort.
In previous studies, the authors used the example of a patient undergoing iodine-131 metaiodobenzylguanidine (I-131 MIBG) dosimetry to show the value of a patient-specific phantom. The research concluded that the tumor's geometry had a significant effect on dose quantification, and that optimization of imaging and dosimetry protocols for specific patients was necessary (European Journal of Nuclear Medicine and Molecular Imaging, October 2011, Vol. 38, Issue 2 Supplement, pp. S435-S435; European Journal of Nuclear Medicine and Molecular Imaging, October 2007, Vol. 34, Issue 2 Supplement, pp. S178-S178).
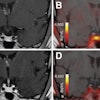
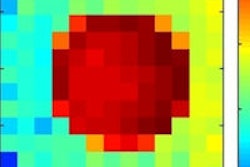
So, for this study, initial scans of the phantoms were performed with technetium-99m SPECT and FDG-PET/CT. Gear and colleagues gathered specifications for the phantom by segmented liver, spleen, and kidney volumes from CT images of a half-body PET/CT scan with no contrast. Each organ was converted to a shell, and holes and leg supports were configured using computer-aided design (CAD) software before printing.
Perfecting the phantom
The researchers continued to develop the design of the phantom by using a 3D surface mesh to remove CT pixelation. The mesh was then smoothed to remove any additional imperfections and each organ was converted to a shell with wall thickness of 2 mm. Adjustments also were made so the inner volume of the shell remained consistent with the volume of the organs.
The team saved the mesh's configuration as a binary stereolithography (STL), which was imported into Autodesk meshmixer software for additional adjustments before printing.
The phantoms were printed from an ultraviolet curable photopolymer using polyjet technology on a 3D printer (Eden 500V, Objet). According to the study, the printer features stereolithography and inkjet technology, while an ultraviolet laser cures the resin to solidify the pattern traced on the tray. The process is repeated for each layer.
"The design of the phantom fulfilled the requirements that the anatomical detail replicated the patient geometry and offered more flexibility for insert placement than commercially available designs, yet allowed reproducible construction on reassembly," they added.
Given the early success of this phantom, Gear and colleagues are optimistic about the reproducibility of the device and future use of the technology.
"As the phantom is designed using CAD, further copies can be easily made with modifications to the design as necessary to suit specific requirements," they wrote. "Further advances in this technology promise to offer more flexibility in design at a reduced cost compared to traditional phantoms and could become a more routine method of phantom manufacture."
Support for the study came from the National Institute for Health Research Royal Marsden/International Congress of Radiology Biomedical Research Centre.