A U.K. audit has found troubling results regarding the accuracy of nontrauma CT abdominal reporting for emergencies outside of normal working hours. Teleradiologists were three times more likely to produce a report with a discrepancy in it, potentially putting patients at risk, according to a 5 December study in Clinical Radiology.
The U.K.-wide audit included almost 5,000 patients scanned in 2013 drawn from many of the acute hospitals in the country. The research team compared radiology subgroups and found teleradiologists working for outsourcing companies had a statistically significant increased risk of major discrepancies, or errors.
"These findings give cause for concern and should provide impetus for further consideration of optimal models of service provision for the reporting of emergency abdominal CT," wrote lead study author Dr. David Howlett, PhD, and colleagues. "It is clear that both the seniority and location of the reporter can have a significant effect on the accuracy of emergency CT reporting and, hence, patient outcomes."
Howlett is a consultant radiologist at East Sussex Healthcare National Health Service (NHS) Trust and honorary clinical professor of radiology at Brighton and Sussex Medical School.
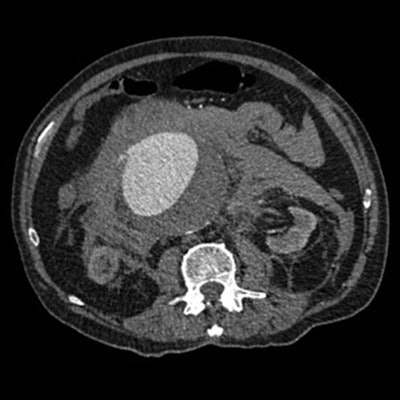
 An example of a CT image of a leaking abdominal aortic aneurysm. Image courtesy of Dr. David Howlett.
An example of a CT image of a leaking abdominal aortic aneurysm. Image courtesy of Dr. David Howlett.The problem with abdominal CT
Acute abdominal pain outside of the trauma setting is common in the emergency department, with a wide spectrum of underlying causes for which CT is used as an integral part of surgical triage, the authors noted.
The rapid increase in CT use, particularly out of hours, has created reporting pressures within the U.K. and has led to the development of different reporting models. Provisional (initial) CT reports may be issued by trainee radiologists (registrars) with subsequent review by senior onsite consultant radiologists, or reports may be issued by consultants themselves. Alternatively, reporting may be carried out by teleradiologists working offsite with no affiliation to the department where the imaging occurs.
Both registrar and offsite reports may be supplemented by an addendum report provided later by an onsite consultant, according to Howlett and colleagues.
"Emergency abdominal or abdominopelvic CT performed out of hours in acutely ill patients is a complex investigation with the potential to impact positively or negatively on patient outcomes depending on the accuracy and timeliness of the report," they wrote.
In the audit, they sought to determine how well radiologists are reporting abdominopelvic CT in surgical and nonsurgical groups by assessing major and minor discrepancy rates for provisional and also addendum reports in patients across a wide range of institutions.
"We undertook the audit originally as there was feedback from fellows of the RCR [Royal College of Radiologists] that there were a large amount of reporting errors in outsourced, on-call reports issued by doctors reporting for teleradiology companies," Howlett wrote in an email to AuntMinnieEurope.com. "This seemed to be a particular problem in the CT abdomen, which is a complex area. So I guess we had a suspicion the audit might throw up some issues, but I was surprised at what we found."
Targets achieved and not achieved
For their study, the researchers defined a major discrepancy as a change, or potential change, in diagnosis or treatment as a result of either the addendum report or CT auditor review, and a minor discrepancy consisted of minor issues in provisional and addendum reports unlikely to result in harm or a change in management. Harms included death or unnecessary intervention, such as colonoscopy, endoscopy, or drainage. A delay in diagnosis or treatment also was considered a harm.
The study included 4,931 patients, of which 2,568 were surgical and 2,363 were nonsurgical. The researchers found the audit standard for major discrepancies in provisional reports was achieved for registrars, onsite consultants, and consultant addenda. However, teleradiologists failed to meet the standard target of less than 5%, achieving 8.7% overall and 12.7% in surgical patients. The standard for patients coming to harm also was not met in the surgical group (target < 1%, achieved 1.5%) and was narrowly missed overall (target < 1%, achieved 1%).
| Major discrepancy rate for provisional reports | |||
| Target | Achieved | ||
| Registrars | < 10% | 4.6% | |
| Onsite consultants | < 5% | 3.1% | |
| Consultant addenda | < 5% | 2.9% | |
| Teleradiologists | < 5% | 8.7% | |
In the nonsurgical group, 47 patients had evidence on notes/imaging review of subsequent additional procedures that may have been unnecessary following a major discrepancy -- predominantly additional imaging procedures, but they also included CT/ultrasound-guided drainage (three patients), laparoscopy (three patients), and endoscopy (three patients). Also, 15 of 72 patients with provisional reports of major discrepancies were considered by the auditor to have come to harm as a result of the report: delay in diagnosis (seven patients), delay in treatment (seven patients), unnecessary investigations (two patients), and unspecified (one patient).
In the surgical group, 36 of the 132 patients with provisional reports of major discrepancies were considered by the auditor to have come to harm as a result of the report: delay in diagnosis (three patients), delay in surgery (24 patients), unnecessary investigations (one patient), and unnecessary surgery (eight patients).
"When compared to an onsite consultant, there was a statistically significant increased risk of major discrepancy and major discrepancy with harm in an offsite/outsourced CT report; this finding was consistent in both surgical and pooled data," the researchers wrote. "Major discrepancy was also found to be more likely in the surgical group."
What to do?
"The best solution to both in- and out-of-hours reporting is ... a consultant, or appropriately supervised trainee radiologists, working onsite; namely, where the patient is imaged," Howlett wrote. "For a number of reasons over the past 10 years or so, the amount of imaging needing reporting has far outstripped the number of reporting consultant radiologists in the U.K., and trainee radiologist numbers have not been expanded. This has meant that other solutions have been explored."
Teleradiology has become popular in the face of this, particularly as the radiology crisis in the U.K. worsens. However, it's expensive -- costing around 88.2 million pounds (105 million euros) in 2015 and likely more this year, and there are quality issues.
"If you talk to clinicians in most hospitals, they are concerned about the quality of many outsourced reports -- needing to get them routinely checked by onsite consultants," he said. "An increased discrepancy rate has been shown on our paper, albeit in a relatively niche but clinically important area. Is this finding replicated across the board in other areas?"
Outsourcing reporting is not a problem per se, but teleradiologists do not have access to patient records, prior imaging, and supporting information from clinicians, so in some ways they are working with their hands tied behind their back. Also the teleradiologists are dealing with often complex studies from multiple specialties outside their general field of knowledge, Howlett said.
"No one, particularly the RCR, is antioutsourcing, and indeed the outsourcing companies have fulfilled a vital role in plugging the current gap between existing onsite reporting resources and demand," he said. "There is no suggestion that outsource reporters are in any way worse radiologists than onsite reporters. Indeed they are often one and the same -- onsite day job, outsource at nighttime/weekend."
What's the answer? Urgent and major investment in training more radiologists, Howlett said. Also, structure how organizations work with outsourcing while staffing levels are addressed, he added.
"My view is [teleradiologist companies] also need to look at their reporting structures and practices, certainly to subspecialize reporters and look at their working hours," he added. "We need to work with them collaboratively on future potential audits to look at discrepancy and value of reports to clinicians across other disciplines such as oncology."