The European Society of Breast Imaging (EUSOBI) and 30 national breast radiology bodies have released a position paper in a bid for clarity on breast cancer screening and digital breast tomosynthesis (DBT). The group's top priority is double-read, biennial mammography for women 50 to 69 years old, but it urges everybody to prepare for screening with DBT.
 Dr. Francesco Sardanelli.
Dr. Francesco Sardanelli.The goal of the paper is to achieve some clarity in the roiling debate over who should receive breast screening, according to lead author Dr. Francesco Sardanelli from the department of biomedical sciences for health at the University of Milan, who is also past president of EUSOBI (European Radiology, 2 November 2016).
"After many years of confusion about the balance between advantages and disadvantages of screening mammography (also in the medical community), this position paper proposes very simple points to women, physicians, and makers of health policies," he wrote in an email to AuntMinnieEurope.com. "Moreover, we tried to present a scheme that can be generally applicable in all countries, with scales of priorities for both technology and age intervals of female population to be covered."
The priorities
There has been much back and forth in recent years about the effectiveness of breast cancer screening. With the new paper, EUSOBI and multiple national bodies have come out on the side of mammography screening, along with providing recommendations for effectiveness. Participating in the paper are 30 national breast radiology groups, from Austria, Belgium, Bosnia and Herzegovina, Bulgaria, Croatia, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Republic of Ireland, Italy, Israel, Lithuania, Moldova, the Netherlands, Norway, Poland, Portugal, Romania, Serbia, Slovakia, Spain, Sweden, Switzerland, and Turkey.
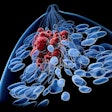
The paper notes that mammography is a proven technology for reducing deaths from breast cancer, despite questions about its effectiveness.
"Notwithstanding its intrinsic limitations in terms of sensitivity and specificity, mammography remains the main tool for population-based mass screening with demonstrated effectiveness in reducing mortality and allowing for conservative treatment," Sardanelli and colleagues wrote.
The paper's first recommendation is biennial screening mammography for average-risk women 50 to 69 years old. Their second priority is extending screening for women up to the age of 73 or 75.
"The incidence of breast cancer is increasing with age and does not stop at 70," Sardanelli wrote in his email. "Evidence does exist (in term of mortality reduction) in favor of this extension to be faced with epidemiological issues such as concurrent causes of death and, as a consequence, overdiagnosis."
Because women are living longer, it makes sense to extend the age for breast cancer screening, he said. "I personally agree with the qualified recommendation from the American Cancer Society to continue screening mammography as long as women's overall health is good and they have a life expectancy of ≥ 10 years. This means, in Italy, to go also over 75," he added.
The third priority for the authors is to screen women ages starting from between 40 and 45 up to 49 annually.
"The incidence is generally lower than after 49 and the evidence in favor of screening mammography in this younger age range is 'limited.' The range 40 to 45 is given to allow for adaptation to local situations," Sardanelli said. "In fact, from 40 to 49, if screening mammography is proposed, it should be performed annually, not biennially, increasing costs and organizational problems."
Epidemiological data show the first relevant increase in incidence in the general average-risk female population happens after 44, thus creating the possibility to start screening at 45 instead of 40.
"In other words, extension from 45 to 49 is the third priority, from 40 to 44 the fourth priority," he said. "Each country, each local screening program could decide this taking into account local issues."
Other priorities for the group include dedicated pathways for high-risk women offering breast MRI according to national or international guidelines and recommendations.
"High-risk women should be included in the organizational strategy of screening programs," Sardanelli wrote. "Already, from 40 to 49, the general old rule 'biennial screening for all' has been changed because in this age range annual screening is needed. High-risk women need an MRI from 25 or 30. Thus, the 'one size fits all' era is over."
In terms of technology, the group encourages adoption of digital mammography -- not film-screen or phosphor-plate computer radiography (CR).
Also, DBT is set to become "routine mammography" in the screening setting in the near future.
The future includes DBT
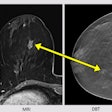
The societies also took into consideration the increasing evidence in favor of DBT as a screening tool. Recent studies have found DBT used as an adjunct or alternative to 2D digital mammography allows for a superior diagnostic performance when compared with 2D mammography alone.
Overall, DBT increases the detection rate from 0.5 to 2.7 per 1,000 screened women and reduces the recall rate from 0.8 to 3.6 per 100 screened women, the societies noted. Also, "DBT is now proposed along with synthetic 2D views, practically solving the problem of an increased radiation exposure when DBT is performed as an adjunct to 2D digital mammography," they added.
The evidence points to DBT becoming routine in the screening setting, but before introducing DBT in the breast cancer screening setting outside of trials approved by ethical committees, there's a need for a statistically significant and clinically relevant reduction in the interval cancer rate, the societies stated.
"This cautiousness is due to the need to avoid an increase in overdiagnosis and costs, in the absence of the demonstration of cost-effectiveness of screening DBT (proof of which may require very long studies)," they wrote. "Moreover, the probable increase in reading time associated with the use of DBT in screening and its effects on sustainability of screening programs should be considered before routine implementation."
"We did not say 'screening with DBT now' because we still need robust evidence of reduction of interval cancers, not to risk an unwanted increase in overdiagnosis. It's quite probable that this evidence will be available in the near future," Sardanelli noted. "Thus, our message is, 'Be ready for screening with DBT.' In other words, if you are planning to purchase new equipment for mammography, including DBT is strongly suggested."