Urgent action is required because a significant number of the 183 radiology departments in the U.K. National Health Service (NHS) do not have a future CT replacement plan in place, and there is a distinct lack of training about dose optimization, according to a major survey involving the Royal College of Radiologists (RCR).
"All NHS radiology departments need a future equipment plan, looking forward at least five years. Professional bodies working together could produce a template or framework to assist these to be developed," the authors noted. "Understanding of dose reduction technologies appears to be poor, and application of these important techniques may be incomplete."
Formal programs to ensure maximum adoption of dose optimization and reduction technologies throughout the NHS may be needed and would help to address public concerns about radiation dosages, they added.
The survey of NHS radiology departments was conducted by the Clinical Imaging Board, collaboration between the RCR, Institute of Physics and Engineering in Medicine, and the Society and College of Radiographers (SCoR). It found that no funded replacement plans were in place for about 40% of CT scanners and some machines have no technology to minimize the x-ray dose received by the patient. More than 10% of respondents said their CT machines did not have the necessary technology to do this effectively.
"There is anecdotal evidence that in the U.K., investment in CT equipment is declining, which may be due to NHS funding restrictions," the authors stated. "There is much pressure to 'sweat the assets,' operating services for longer hours and increasing throughput, to help make access to diagnostic tests ever more speedy. While all of these goals are clinically imperative, the U.K. operates CT scanning from a very low installed base of less than nine scanners per million population."
The e-questionnaire asked the local CT lead radiographer to respond to a series of questions and provide data about each CT unit at their hospital. The survey was promoted at the SCoR's National Conference for Radiology Managers meeting in May 2014, and through the society's Synergy News magazine.
There were 117 responses, giving information about 298 CT scanners. A total of 208 machines were owned by the NHS, 30 were leased, 54 obtained as part of a managed equipment service, and there were six "don't know" responses. The mean age of CT equipment was 4.8 years. This suggests that average equipment age had improved since a National Audit Office survey was carried out in 2011.
Around 62% of respondents have replacement plans in place, some of which include funds already committed. Where used, managed equipment services also provide clear timelines for future replacement. No replacement plans are in place for 112 scanners, and 13 respondents said they don't know.
The survey shows a steady procurement rate of about 30 machines per year. As the chart shows, there appears to be a decline in replacement over recent years, and this is probably due to less-certain planning further into the future, according to the report.
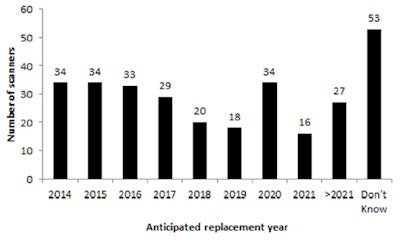 Future replacement CT numbers planned by year.
Future replacement CT numbers planned by year.Average annual CT growth is 10.3% per annum since 2003, while the overall growth rate for imaging is 3.3%. Only MRI, growing at an average of 12% per annum since 2003, is increasing at a rate faster than CT. CT use increased in England by 13% to 3.8 million examinations in 2013-14, and demand for CT grew faster than MRI during this period. Based on annual midyear population statistics published by the Office for National Statistics, this equates to 71.3 CT studies per 1,000 population.
Comparing with the most recent data available for Organization for Economic Cooperation and Development (OECD) countries,10 CT exams per 1,000 population elsewhere in the world range from 29.1 (Finland 2012) to 240.2 (U.S. 2013). Across a basket of 18 OECD participant nations, mean CT usage rates in 2012 were 125.1 per 1,000 population, meaning U.K. use is only 57% compared with the other countries.
The survey indicates that only 110 (37%) of CT units have automatic tube current modulation (ATCM) technology and 24 (8%) have iterative reconstruction capability. However, the authors suspect that few responders were aware of the dose reduction terminology used in the questionnaire and may have given incorrect replies. Most of the installed CT base in the U.K. will have ATCM technology, they pointed out.
Furthermore, a wide variation in throughput exists, and is not directly related to hours of operation (see chart). A small proportion of scanners appear to be used much less than others. This may relate to a particular case-mix, or to patient referral patterns, and so is a finding that must be viewed with caution, they emphasized.
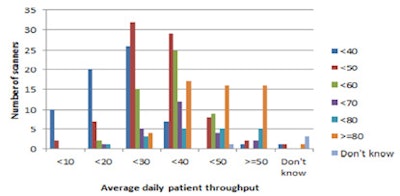 Average daily throughput by frequency, with additional color coding for patients per day.
Average daily throughput by frequency, with additional color coding for patients per day."Weekly hours of operation and patient throughput varies widely between machines and organizations. This will demand additional equipment or working longer clinical hours. Additional staff will be required to support this both to undertake the imaging and to provide the requisite reporting," the authors wrote.
Most scanners are used for a wide range of "specialist" applications from cancer scanning, through to angiographic and cardiac applications as well as CT colonography. Utilization of CT equipment to acquire cardiac imaging is lowest at only 33%.
Overall, the specification of the U.K.'s CT equipment is high, with only 26% of equipment being below 64-slice capability.
"There is a small proportion of CT equipment (11%) still in clinical use well after its recommended end of life. NHS organizations should ensure this equipment is well maintained and that patients have alternative access to current technology equipment where needed within an NHS trust or across a network through partnership arrangements," they noted.
The age profile of U.K. CT equipment still does not compare favorably with other European countries and there is a risk that due to current economic pressures within the NHS that equipment replacement may become more challenging, they continued.
There is a need to raise awareness of the low numbers of CT scanners per million population in the U.K. compared with many other similar countries, the authors concluded. With more than 10% of CT equipment being more than 10 years old and not having dose optimization capability, this creates inequity for patients and action is need to address this situation.