Researchers from Hong Kong have determined that digital breast tomosynthesis (DBT) had higher sensitivity and better characterized more lesions than full-field digital mammography (FFDM) and synthesized 2D mammography when screening women at moderate risk of breast cancer.
The ongoing, prospective study compared the lesion detection and characterization ability for both malignant and benign masses for FFDM, synthesized 2D mammography, and DBT. The researchers from Queen Mary Hospital also evaluated differences in radiologists' confidence levels when using the three modalities, finding DBT comes out on top with a sensitivity of 91.8%.
The research team, led by Dr. Lorraine Sinn from the department of radiology, found that DBT was better at characterizing which masses would turn out to be benign or probably benign, and radiologists reading DBT images had higher confidence levels for images with malignant masses compared with those reading FFDM images.
Just how good is DBT?
DBT has already proved its superiority to FFDM in multiple studies. Recent research has also focused on comparing FFDM to synthesized 2D mammography, in which synthesized 2D images are created from 3D datasets acquired with DBT. The hope is that synthesized 2D images could be used with DBT to eliminate the need for a 2D image acquired with conventional FFDM, thus lowering radiation dose.
However, most recent studies have focused on DBT's impact on cancer detection and recall rate. Instead, Sinn and colleagues wanted to focus on DBT's ability to characterize suspicious lesions, as well as its impact on radiologist confidence levels when reading images. They presented their work at ECR 2016.
Starting in October 2014, the study included women undergoing their annual mammography screening at Queen Mary and who had a moderate risk of developing cancer. Study participants included women older than 40 who were called back for further assessment after a routine screening exam, as well as women with other risk factors such as a previous personal or family history of breast cancer.
Two-view FFDM and two-view DBT were performed in the same setting. Synthetic 2D mammograms were created from the DBT data. Nine radiologists reviewed the FFDM, DBT, and synthetic 2D mammography images without access to prior examinations or clinical history.
 Diagram shows the craniocaudal view of left breast of the same patient in FFDM, synthesized 2D mammography, and selected DBT slice. There is an irregular mass noted at lateral aspect where the spiculations are much easier appreciated by DBT. This lesion was only depicted by DBT and missed by FFDM and mammography during images review. Lesion was a histologically proven invasive ductal carcinoma. All images courtesy of Dr. Lorraine Sinn.
Diagram shows the craniocaudal view of left breast of the same patient in FFDM, synthesized 2D mammography, and selected DBT slice. There is an irregular mass noted at lateral aspect where the spiculations are much easier appreciated by DBT. This lesion was only depicted by DBT and missed by FFDM and mammography during images review. Lesion was a histologically proven invasive ductal carcinoma. All images courtesy of Dr. Lorraine Sinn.Histological proof was the gold standard for differentiating malignant from benign lesions. In the case of no histological proof, ultrasound or MRI was used to problem-solve. A mass was considered "probably benign" when correlated with ultrasound or MR images performed in the same session or the same year. The lesion was also classified as probably benign if it was static compared with previous mammograms and also within the follow-up period.
As in the evaluation of suspicious masses, histological proof was the gold standard.
The researchers included 473 women with a mean age of 56.1, resulting in 767 datasets (multiple images were taken from the same women).
In terms of detecting benign or probably benign lesions, FFDM detected 102 lesions, synthetic 2D mammography detected 85, and DBT detected 125. For suspicious lesions, FFDM detected 11, synthetic 2D mammography detected 13, and DBT detected 15.
DBT also demonstrated sharply higher sensitivity than the other two modalities.
| Comparison of FFDM, synthesized 2D mammography, and DBT | |||
| FFDM | Synthesized mammography | DBT | |
| Sensitivity | 69.0% | 65.5% | 91.8% |
| Specificity | 94.7% | 96.3% | 94.8% |
| Positive predictive value | 64.5% | 67.9% | 68.3% |
| Negative predictive value | 93.4% | 94.6% | 97.9% |
The researchers also measured the confidence level of the radiologists when they saw a lesion using a five-point scale, with 1 being least confident and 5 being very confident. In 45 lesions in which they were detected in all three modalities, radiologists had higher confidence levels in 45% of cases reading DBT images compared with those reading FFDM images. In all, the researchers were more confident using DBT, with an average increase of 1.23 points.
"Our study shows that for those lesions that were detected by all three modalities, the interpreting radiologists were more confident in calling the lesions in 45% of them compared to FFDM," Sinn said in an interview with AuntMinnieEurope.com. "In short, it improves the diagnostic confidence."
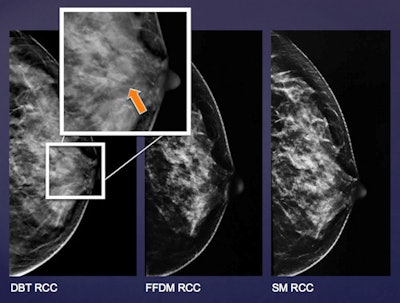 Diagram shows the left breast of the same patient in FFDM, synthesized 2D mammography, and selected DBT slice. There is a well-defined low-density mass noted at the retroareolar region, which was only depicted by DBT but not by FFDM and mammography during image review. Lesion was confirmed to be a fibroadenoma on subsequent ultrasound with fine-needle aspiration performed.
Diagram shows the left breast of the same patient in FFDM, synthesized 2D mammography, and selected DBT slice. There is a well-defined low-density mass noted at the retroareolar region, which was only depicted by DBT but not by FFDM and mammography during image review. Lesion was confirmed to be a fibroadenoma on subsequent ultrasound with fine-needle aspiration performed.When comparing the lesions with each other, only three out of 13 additional occult lesions in FFDM and two out of six additional occult lesions in synthetic mammography were confirmed to be benign or probably benign lesions. Meanwhile, 32 additional lesions were found only by DBT, 75% of which were confirmed to be benign lesions.
"We are more accurately diagnosing those lesions which are underdiagnosed by FFDM," Sinn said.
What's more, most (75%) of the lesions detected only by DBT turn out to be benign on subsequent imaging follow-up and imaging, while for lesions detected only by FFDM, only three out of 13 (15%) turned out to be benign.
"Hence, FFDM is actually overdiagnosing in that sense instead of DBT," Sinn said.
The findings are particularly important, because before synthetic 2D mammography, radiologists had to perform FFDM in addition to DBT, thus resulting in a higher radiation dose. With synthetic 2D, that is no longer an issue.
"Thus, in Asian women, when synthesized 2D mammography is used in lieu of FFDM, it is going to retain the superiority of DBT, with the 2D information that is adequately comparable with FFDM, and yet with a significantly lower radiation dose than FFDM," Sinn said.
Limitations and next steps
The study does have some limitations, however. Namely, not all patients had ultrasound performed in same setting or within the same year. Also, not all lesions detected by mammography were detected by ultrasound. In addition, this was a single-reader study with limited data to date.
Sinn's group has plans for future research, including a more extensive comparison on the diagnostic performance of the three modalities in women with different breast densities. The researchers are planning to omit the FFDM for diagnostic use and completely replace it with synthetic mammography in the near future, and they would even like to see if DBT can obviate the need for ultrasound as a follow-up tool, as it has already done with FFDM.
"DBT significantly reduces the need for additional views in our clinical practice," Sinn said.