Norway's breast cancer screening initiative has reduced mortality by 20% to 30% for women ages 50 to 69, followed to age 79, when compared with no screening, indicated figures released by the Research Council of Norway.
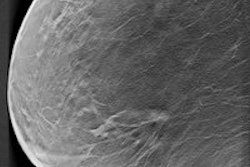
There has been fierce debate over whether screening mammography's benefits outweigh its harms. In a report titled "Research-based evaluation of the Norwegian Breast Cancer Screening Program," submitted to the Ministry of Health and Care Services on 12 June, evidence continues to mount that breast cancer screening does lead to significant reductions in mortality. However, each woman needs to decide for herself as well.
"From a societal perspective, recognizing the uncertainty of the estimates, the cost-effectiveness of the program seems to be within the range of what Norwegian Health Authorities define as acceptable for health services," the council wrote. "On the individual level, however, each invited woman has to weigh the information on potential benefits and harms based on her own values, health, and life situation when deciding on whether or not to attend the program."
Does screening do what it should?
The council, chaired by Dr. Roar Johnsen from the Norwegian University of Science and Technology in Trondheim, conducted the evaluation of the Norwegian Breast Cancer Screening Program (NBCSP). The evaluation was based on observational studies and lasted from 2007 to May 2015.
The aim was to investigate whether NBCSP fulfills its intentions and purpose, in this case a target of 30% mortality reduction. In Norway, all women ages 50 to 69 are invited for mammography screening every two years. The program was launched as a pilot project in four counties between 1995 and 1997 and went national in 2004. The stepwise process meant the council could compare women invited for screening with those not invited. A special registry provides information on the date of exposure and attendance, as well as the results of mammograms.
The committee decided to have at least two different project groups to assess breast cancer mortality, overdiagnosis, and health economics; the two groups had the same sets of data from a common project database. It concluded that NBCSP reduces mortality by 20% to 30%, the reason for the range being that studies are conducted with very different designs and analytical approaches.
"There was no defined plan for an evaluation of the program when nationwide implementation was decided," the authors wrote. "Thus, there were no predefined intervention and control populations where prior knowledge about important influencing factors had been taken into consideration."
Such factors include regional and temporal differences in breast cancer risk and mortality, nonprogram screening, and use of hormone therapy.
"If information on the expected influencing factors had been systematically collected at an individual level and regardless of screening invitation or attendance status, this would have helped the evaluation considerably," they added. "Furthermore, the implementation of the program coincided with important trends in modern multidisciplinary diagnosis and treatment of breast cancer. In consequence, based on observational studies, the evaluation could not fully distinguish between the effects of the NBCSP and the effect of multidisciplinary management."
Risk of overdiagnosis
When mammography screening is criticized, it's usually due to overdiagnosis. For women ages 50 to 79, the most reliable estimates of overdiagnosis for invasive breast cancer and ductal carcinoma in situ (DCIS) combined were in the range of 15% to 25%, compared with no screening. For women ages 50 to 79 in a situation with screening, the council considers the corresponding estimates to be in the range of 15% to 20%. The reasons for uncertainty in the estimates are the same as for mortality reduction and, additionally, the use of different denominators.
"The committee considers that a somewhat higher estimate of overdiagnosis in the Norwegian program, compared to estimates from reviews of the mammography screening trials, may be associated with a higher sensitivity of the Norwegian program," noted the authors. "We emphasize that the uncertainty in these estimates is considerable."
In absolute numbers, among 10,000 women invited for screening (at age 50) and screened 10 times, approximately 27 breast cancer deaths would be avoided at a price of 142 overdiagnosed breast cancers, or for each breast cancer death prevented, approximately five women are overdiagnosed. However, an overdiagnosed breast cancer would be expected to need less aggressive treatment, cause less harm, and generate lower additional costs than an additional clinically detected breast cancer, they stated.
Costs
The societal costs of one screening round was 1,389 Norwegian krone (158 euros) per woman attending screening in 2012, including the costs of recalls after positive mammography.
The estimated 10-year treatment costs for breast cancer were 356,000 Norwegian krone (around 40,680 euros) measured in 2008 prices.
The cost per quality-adjusted life year gained was estimated to be 190,000 Norwegian krone (21,710 euros) to 479,000 (54,720), which is in the lower part of the range used by the Norwegian Directorate of Health for cost thresholds (400,000-1,000,000 Norwegian krone per life year gained).
The council is organizing a national conference to be held on 7 September, where one of the topics will be the evaluation results. Click here for more information (in Norwegian).