An interesting dialogue has developed on the worth of maximum standardized uptake values (SUVmax) from FDG-PET/CT scans to accurately diagnose mediastinal lymph nodes in patients with non-small cell lung cancer (NSCLC).
In an editorial published online on May 16 in the European Journal of Radiology, Italian researchers are questioning conclusions from a study performed by Cork University Hospital in the Republic of Ireland that used SUVmax thresholds and various ratios to measure and determine the extent of mediastinal disease in NSCLC patients.
"The possibility to reduce variability using SUV ratios ... is interesting," wrote lead author Dr. Valentina Ambrosini, from Sant' Orsola Hospital at the University of Bologna School of Medicine, and colleagues. "However, larger studies are needed to better ascertain their value and the possibility of their introduction in daily clinical practice" (EJR, 16 May 2014).
The Irish perspective
The retrospective Irish study was led by Dr. Fiachra Moloney from the department of radiology at Cork University Hospital. Researchers reviewed patients with NSCLC and mediastinal nodes using an SUVmax in the range of 2.5 to 4.0 on FDG-PET/CT scans (EJR, 24 February 2014).
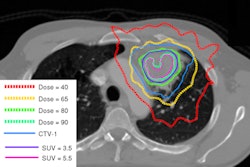
The researchers analyzed a total of 92 mediastinal lymph nodes in 44 patients, with stage 2 and stage 3 mediastinal disease confirmed in 15 (34%) of 44 patients and in 34 (37%) of 92 lymph nodes. Positive predictive value was 37%, and the false-positive rate was 63%.
In the true-positive cases, the researchers found lymph node SUVmax, tumor size, the ratio of node SUVmax to tumor SUVmax, and ratio of node SUVmax to node size all were significantly greater.
When Moloney and colleagues used a threshold of 0.3 for the SUVmax node/tumor ratio, they achieved sensitivity of 91% and specificity of 71% for detecting mediastinal disease. When a threshold of 3.0 was used for the SUVmax node/size ratio, sensitivity was 71% and specificity was 69% for mediastinal disease detection.
When both ratios were combined, sensitivity was 65% and specificity was 88%. In addition, concurrent benign lung disease was observed significantly more frequently in false-positive cases.
Hence, Moloney and colleagues concluded that the two ratios "may be complementary to conventional visual interpretation and SUVmax measurement in the assessment of mediastinal disease in patients with NSCLC."
Italian counterpoints
FDG-PET/CT has long been used to routinely evaluate the metabolic activity of cancer cells by reflecting the activity of glucose metabolism as it increases with active cells. The greater the FDG uptake, the greater the chance a node is malignant. That ability to detect early malignancies is critical in selecting appropriate clinical treatment and therapeutic options for patients with NSCLC.
Based on other published literature, however, Ambrosini and colleagues offered a different view, asserting that using SUVmax thresholds greater than 2.5 to differentiate benign and malignant lesions is "invalid." They noted that many active inflammatory/infectious processes may show a high SUVmax value, while low FDG uptake may be seen in slow-growing neoplasms and scarcely to non-FDG-avid tumors, or SUVmax determination may be inaccurate in cases of small lesions due to partial-volume effect.
The researchers also cautioned that the Irish study had a limited patient cohort with a relatively high number of patients presenting with chronic benign lung disease and a neuroendocrine tumor with lower FDG avidity. "Therefore, further investigations in larger samples are needed to confirm their findings," Ambrosini and colleagues wrote.
They also noted that current guidelines for lung cancer management suggest an invasive procedure to accurately stage patients presenting with positive mediastinum nodes seen on CT or PET/CT, or when physicians have a high suspicion of nodal metastasis.
"SUVmax is certainly an interesting parameter to study that can provide valuable clues regarding the nature of a suspect lesion," Italian researchers added, "however, it should be interpreted taking into account the pretest probability of malignancy, morphological imaging findings, and only when standardized measurement has been performed."
While the possibility to reduce variability using SUV ratios is "interesting," Ambrosini and colleagues wrote, "larger studies are needed to better ascertain their value and the possibility of their introduction in daily clinical practice."