The U.K. Royal College of Radiologists (RCR) has published updated recommendations for cross-sectional imaging in cancer management. They can be downloaded free of charge from the RCR's website.
The new second edition (Ref No: BFCR[14]2) takes over from the first edition, published in 2006. It brings together CT, MRI, and PET within the same document, reflecting the current clinical practice of these complementary techniques. At different points along the patient pathway, one of these modalities may be appropriately used, depending on whether treatment is curative or palliative, and whether the imaging focus is for local or metastatic disease, according to Dr. Pete Cavanagh, the RCR's vice president for clinical radiology.
"These guidelines are intended to provide practical advice and recommendations which should be achievable for the majority of patients. However, they are not intended to be prescriptive and could be adapted readily to meet local requirements," he stated in the preface. "Ultrasound, which has a major role in cancer management, has not been included."
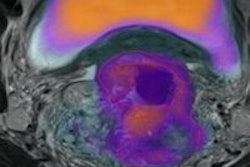
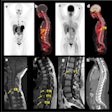
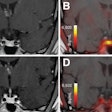
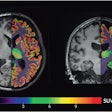
Specific sections deal with imaging in the evaluation of cancer, general techniques for examinations discussing CT, biopsy and MRI, PET/CT, lymph nodes, tumors of the brain, and tumors of the spinal cord.
The authors have tried to follow as closely as possible a standardized page layout, including reference to the tumor node metastasis (TNM) classification, where appropriate, Cavanagh noted. No information on image interpretation has been included because it can be found in textbooks, journals, and Internet resources.
A major advantage of adopting national guidelines is the ability to provide a streamlined effective service in which appropriate scans are undertaken according to the patient's tumor type and purpose of the examination. The new protocols will also ensure that imaging studies can be compared more accurately during follow-up in an individual patient, irrespective of where the patient has been imaged, and this is particularly important for reducing the need to repeat imaging of patients being entered into clinical trials, he explained.
The following steps can help ensure good practice in cancer imaging:
The provision in the request form of all clinical information relating to histological diagnosis, site of known disease, previous surgery or other treatment, and the purpose of the examination. "All cross-sectional imaging requests in patients with known or suspected cancer should be vetted by radiologists or experienced radiographers and priorities for examinations should be set in compliance with local and national guidance," the authors stated.
The timing of the staging investigation after surgery must be considered carefully.
All previous radiological investigations should be available or retrievable in an electronic form for review by the radiologist responsible for the examination.
Each department should have written well-defined protocols for standard examinations, but examinations may need to be tailored to answer specific questions.
Where possible, review examinations before the patients leave the department.
Radiologists should be familiar with the normal range of appearances on their equipment because this varies considerably on different machines, particularly for MRI.
Lymph nodes should be measured in the short axis in the axial plane.
Because response to treatment and disease progression are often assessed according to changes in tumor size, follow-up exams should be performed with comparable technique using the same planes and sequences.
Great variations exist in style of reporting, but it is good practice to provide a structured report with succinct conclusions, paying attention to answering the clinical question posed.
All relevant examinations should be available for review in a multidisciplinary meeting, especially when there is discrepancy between clinical and imaging findings or other diagnostic uncertainty.
In the U.K., more than 2 million patients are estimated to be living with cancer, Cavanagh wrote. The number of people being diagnosed with cancer each year rose from 283,000 in 2011 to 331,487 in 2011. In the 1970s, only 23% of cancer patients survived for 10 years, but by 2007, the figure had doubled to 46%, he stated.
For more details on the guidelines, click here.