The European Society of Urogenital Radiology (ESUR) has updated its guidelines regarding acute abdominal and pelvic pain during pregnancy. The group found that ultrasound and MRI are still the preferred modalities for this indication, among other conclusions.
There are diagnostic and therapeutic challenges associated with acute abdominal pain during pregnancy -- namely, the diagnosis is confounded by several common features of normal pregnancy, including nonspecific pain, nausea, and vomiting. Clinical examination is more difficult, and there is also displacement of abdominal and pelvic structures by the gravid uterus (European Radiology, 30 August 2013).
"Prompt diagnosis and treatment are essential for the well-being of the mother and the fetus, and imaging is commonly requested to clarify the clinical picture and expedite diagnosis," wrote Dr. Gabriele Masselli, from the department of radiology at Policlinico Umberto I Sapienza University Rome, and colleagues. "Given the established risks to the fetus from radiation exposure, ultrasound and magnetic resonance imaging are the strongly preferred imaging investigations."
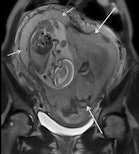
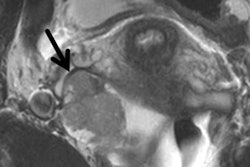
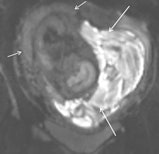 Subchorionic hemorrhage due to placenta abruption in a 30-year-old woman at 29 weeks gestation presented with acute pelvic pain and vaginal bleeding. Left: Coronal T1-weighted gradient-echo image (4.1/1.1, 10° flip angle) shows a large, hyperintense subchorionic hematoma (arrows). Middle and right: The intrauterine hematoma is mildly hyperintense to placenta on the sagittal T2-weighted half-Fourier RARE image (1000/90) (Middle) and markedly hyperintense to placenta on the sagittal diffusion-weighted image (b value, 800 sec/mm2) (right). Note the hematoma has hypo- and hyperintense areas, due to repeated bleeding. Short arrows indicate the placenta. All images courtesy of Dr. Gabriele Masselli.
Subchorionic hemorrhage due to placenta abruption in a 30-year-old woman at 29 weeks gestation presented with acute pelvic pain and vaginal bleeding. Left: Coronal T1-weighted gradient-echo image (4.1/1.1, 10° flip angle) shows a large, hyperintense subchorionic hematoma (arrows). Middle and right: The intrauterine hematoma is mildly hyperintense to placenta on the sagittal T2-weighted half-Fourier RARE image (1000/90) (Middle) and markedly hyperintense to placenta on the sagittal diffusion-weighted image (b value, 800 sec/mm2) (right). Note the hematoma has hypo- and hyperintense areas, due to repeated bleeding. Short arrows indicate the placenta. All images courtesy of Dr. Gabriele Masselli.Masselli and colleagues on the ESUR Female Pelvic Imaging Subcommittee sought to develop guidelines for the appropriate imaging of acute abdominal and pelvic pain in established intrauterine pregnancy based on a detailed literature review and consensus expert opinion.
The team crafted a questionnaire regarding imaging of pregnant patients presenting with acute abdominal and pelvic pain, then distributed it to all the subcommittee members. The questionnaire evaluated what imaging modalities were used by the members in pregnant patients presenting with acute abdominal and pelvic pain, the clinical indications, and the diagnostic protocols.
Here are the final recommendations that the subcommittee approved during ECR 2013.
Imaging techniques
Ultrasound remains the primary modality because of its availability, portability, and lack of ionizing radiation.
"It often elucidates the cause of abdominal pain, particularly for obstetric or gynecological abnormalities," the researchers wrote. "However, evaluation of the bowel, pancreas, ureter, and mesenteric vasculature may be limited on ultrasound because of altered body habitus, small field-of-view, and the presence of interfering overlying structures."
Also, air within the bowel loops displaced cranially by the uterus can limit evaluation of the mesenteric vessels and pancreas.
MRI is valuable in evaluating specific causes of abdominal and pelvic pain in pregnancy and is the preferred tool when ultrasound is inconclusive, they wrote.
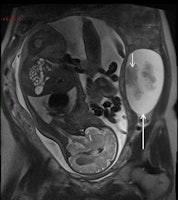
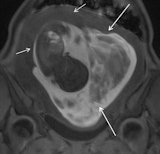
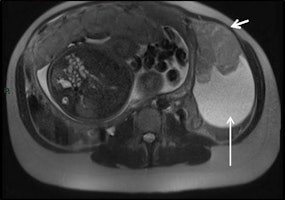 Serous ovarian cystoadenocarcinoma in a 34-year-old woman at 32 weeks gestation presented with acute abdominal pain. Coronal (left) and sagittal (right) T2-weighted MR images show a complex mass, with fluid and solid components (short arrows) on the left ovary.
Serous ovarian cystoadenocarcinoma in a 34-year-old woman at 32 weeks gestation presented with acute abdominal pain. Coronal (left) and sagittal (right) T2-weighted MR images show a complex mass, with fluid and solid components (short arrows) on the left ovary.The modality is particularly helpful when the gravid uterus limits ultrasound. However, MRI poses theoretical risks to the fetus, and care must be taken to minimize these with the avoidance of contrast agents.
Also, breath-hold multiplanar T2-weighted sequences based on a half-Fourier reconstruction technique, balanced gradient-echo sequences, the axial and sagittal T1-weighted gradient-recalled echo sequences, and diffusion sequences are the optimal MR protocols, according to the researchers.
Sometimes neither ultrasound nor MRI is appropriate, particularly in cases of severe trauma. In those instances, "CT cannot be delayed because of radiation concerns," the researchers wrote.
Recommendations for clinical practice
The researchers also detailed what to do in specific situations during clinical practice.
- Placental abruption: MRI should be considered after negative ultrasound findings when there is high clinical suspicion and when a firm diagnosis of abruption would change clinical management.
- Placenta adhesive disorders: Ultrasound for patients with clinical risk factors; proceed to MRI for equivocal cases, especially in patients with posterior placenta and previous myomectomy.
- Uterine rupture: MRI to diagnose antepartum uterine rupture in patients with indeterminate ultrasound evidence, showing the tear itself, and other uterine wall defects, including uterine dehiscence.
- Adnexal mass: Ultrasound can assess most masses; however, MRI can provide further characterization, particularly for evaluating their hemorrhagic content.
- Leiomyoma: Ultrasound is accurate in most cases. Perform MRI if there is any difficulty differentiating from an adnexal mass.
- Ovarian torsion: MRI should be performed after inconclusive ultrasound and can detect hemorrhagic infarction.
- Urolithiasis: Ultrasound is the first imaging test despite its substantial limitations. MR urography (MRU) differentiates physiological urinary tract dilatation from abnormal dilatation related to urolithiasis. In unresolved cases, CT remains a reliable technique for depicting obstructing urinary tract calculi in pregnant women.
- Appendicitis: Ultrasound can be limited by the pregnant body habitus, especially in the later stages of gestation. MR should be performed in cases of inconclusive ultrasound.
A first draft of the guidelines was discussed at subcommittee meetings in 2012, where all the members discussed their judgments during a face-to-face meeting, according to Masselli.