MR enterography (MRE) is both sensitive and specific for the detection of Crohn's disease compared to both endoscopy and histology, and should be used in place of other methods in young patients when it's feasible to do so, according to a study in the European Journal of Radiology. CT works well, but its radiation is a concern in young patients with long lives ahead of them.
For its part, MR enterography costs more to perform than CT enterography, but it eliminates CT's radiation dose while remaining noninvasive and accurate, wrote Dr. David Grand and colleagues from Warren Alpert School of Medicine, in Providence, Rhode Island, U.S., along with colleagues from three local hospitals. The study examined a large cohort of 310 Crohn's disease patients who underwent both colonoscopy and MRE, yielding an overall sensitivity of about 85% for the noninvasive exam. MRI maintained its sensitivity in both distal and ileal Crohn's disease.
"Cross-sectional imaging is currently a mainstay of evaluation of patients with Crohn's disease due to its ability to assess the entire bowel and extraluminal complications including fistula and abscess," Grand and colleagues wrote. CT enterography is the most common examination, but MRE has recently shown excellent efficacy both in detection of Crohn's disease as well as in differentiation of active from chronic small bowel changes, the authors wrote in the article in press (Eur J Radiol, 23 March).
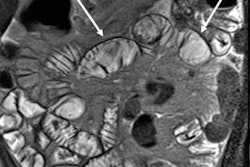
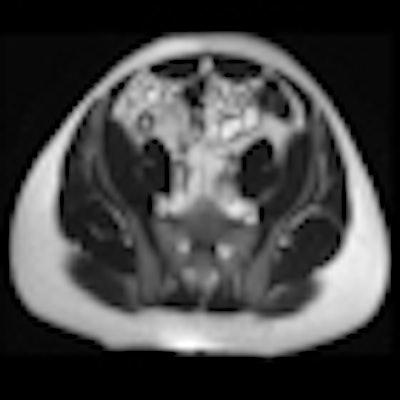
 Patient with mild active terminal ileitis. All images courtesy of Dr. David Grand.
Patient with mild active terminal ileitis. All images courtesy of Dr. David Grand.
Smaller studies consisting of as many as 50 patients have compared MRE to endoscopy in Crohn's disease, but all of them have relied on pharmacologic antiperistaltic agent to minimize the motion artifacts that are a central problem with MRE, especially in contrast-enhanced images, the group noted. However, these add to the cost of the exam and have not been proven necessary in order to produce high-quality images.
As a result the study team decided to forego the use of antiperistaltic agents in the present study, which evaluated the efficacy of MRE in patients with known or suspected Crohn's disease compared to colonoscopy and histology.
The group retrospectively reviewed the records of 850 consecutive patients who underwent routine MRE to evaluate known or suspected Crohn's disease. Of these, 310 patients (171 women, 141 men, ages 20-94, average 45 years) also underwent endoscopy and biopsy within 90 days of MRI.
MRI results were then compared to colonoscopy and pathology reports to determine the presence or absence of disease in evaluable bowel segments. Individual imaging parameters (including wall thickening, enhancement, T2 signal, mesenteric vascular prominence, and adenopathy) were also separately analyzed to determine their independent predictive value, the authors wrote.
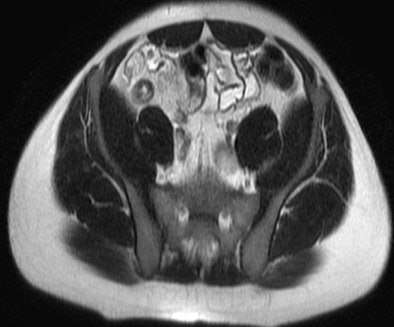
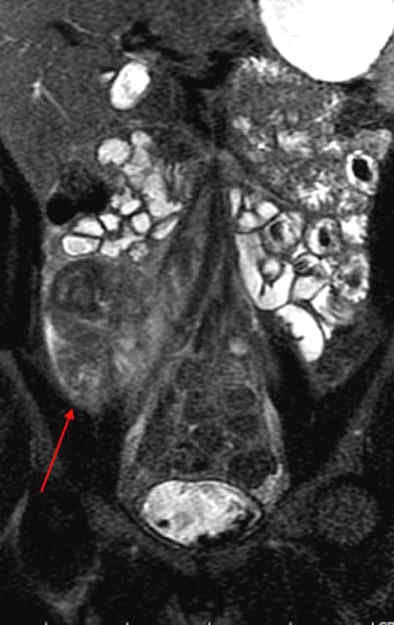
 Patient with long segment terminal ileitis and extensive active inflammation. Note the matted, markedly inflamed ileal loops in the bottom two images.
Patient with long segment terminal ileitis and extensive active inflammation. Note the matted, markedly inflamed ileal loops in the bottom two images.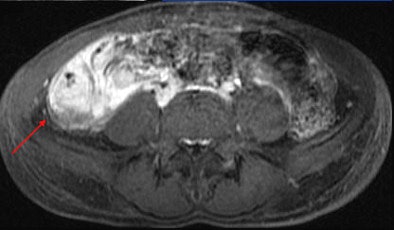

The patients fasted for four hours before ingesting 900 cc of a low-density oral contrast medium (VoLumen, Bracco, Milan) 45 minutes before the scan, in addition to 450 cc of water immediately prior to scanning on a 1.5-tesla scanner from one of three manufacturers.
The study team acquired steady-state free-precession (SSFP) images of the abdomen and pelvis (TR= 4 ms, TE = 2 ms, slice thickness 8 mm for coronal images and 8-mm for axial images). Axial and coronal fat-suppressed half-fourier single-shot fast-spin echo (SSFSE) and axial spoiled-gradient images were also obtained through the abdomen, followed by T1-weighted fat-suppressed spoiled-gradient echo (LAVA/VIBE) images, before the injection of 1 mmol/kg of gadopentate dimeglumine contrast (Bayer Healthcare) followed by a saline flush and postcontrast imaging.
A single experienced abdominal radiologist, blinded to the final results, interpreted all of the MRE images, rating wall thickness, abnormal enhancement, abnormal T2 signal, and mesenteric vascular prominence on a scale of 1-4. All endoscopy reports were reviewed for mention of inflammatory changes in specific bowel segments, and pathology reports were reviewed for the presence of inflammatory disease, the study team reported.
Using endoscopy as the gold standard, MRE results in 310 patients revealed sensitivity of 85% and specificity of 80% overall, Grand and colleagues reported. MRE's sensitivity for the detection of pathologically severe disease was 87% in the terminal ileum and 88% in the colon. The results improved further in the subset of 162 patients who underwent colonoscopy within 30 (rather than 90) days of MRE. In these cases the overall sensitivity remained 85% but the specificity increased to 85% (kappa = 0.69) the study team wrote.
Accuracy of colonoscopy, pathology, and MR enterography in patients undergoing both MRE and colonoscopy within 30 days
|
In the subset of patients who underwent both MRE and colonoscopy within 30 rather than 90 days, specificity was 85% compared to 80% for the entire cohort.
Mild pathologic changes are more difficult to detect with MRE or any other imaging test compared to severe changes, the authors wrote. Thus, the sensitivity of MRE for detection of pathologically mild disease was 68% in the terminal ileum and 27% in the colon, versus 87% in the ileum and 88% in the colon for severe disease. The negative predictive value of MRE was 89% for distal ileal disease and 96% for colonic disease, "indicating that MRE may successfully exclude active Crohn's disease," Grand and colleagues stated.
Interestingly, the results were in line with smaller studies that used antiperistaltic agents, they wrote. As in those studies, MRE showed its real strength in a couple of features of active Crohn's disease. "Analysis of individual MR parameters demonstrates that wall thickening and abnormal enhancement are the most sensitive indicators of Crohn's disease on MRE while abnormal T2 signal, mesenteric vascular engorgement, and adenopathy were insensitive but specific," he wrote.
Limitations include the use of a single, experienced gastrointestinal radiologist to read the MRE, while several experienced readers performed the other exams. While this may introduce variation into the "gold-standard," it accurately reflects daily practice and the ability of MRE to predict changes of Crohn's disease across various clinicians," the authors stated.
It bears noting that neither endoscopy nor pathology are truly adequate gold standards, as MRE evaluates the entire length of the small bowel.
MRE is highly sensitive and specific, and demonstrates excellent agreement with colonoscopy and pathology in a large group of patients who were not given peristaltic agents, the team concluded. It offers valuable information noninvasively, and does so "without exposing the patient to radiation and its potential long term consequences, albeit at a higher initial financial cost compared to CTE," they wrote. MRE should be the standard approach to imaging Crohn's disease in young patients, but CT still has a major role to play.
Nevertheless, "the fact that MR Enterography performs quite well shouldn't sway us to abandon CT enterography," Grand wrote in an email to AuntMinnieEurope.com. "CT enterography is a terrific test and, quite frankly, it's not only more widely available but it is easier to perform and interpret."
For older patients, CT enterography should probably therefore be standard with MR used in its place in younger patients who may require numerous scans throughout their lives, he stated. "The final consideration in the choice of modality is the differentiation of active predominant from fibrostentotic predominant disease and the use of imaging to assist in triaging patients to medical versus surgical therapy," Grand wrote. "MR enterography may prove superior to CT enterography in this regard, but this remains to be proven."