The sensitivity and patient acceptability of CT colonography (CTC) suggest that it's a useful examination for colorectal cancer, but whether screening with the technique is cost-effective will depend on its efficiency in detecting extracolonic findings and on how population-based screening plays out, given the lack of large-scale pilot studies, according to Dutch and U.K. experts.
CTC has several advantages as a primary screening modality, including demonstrated patient acceptability and high detection sensitivity on par with that of conventional colonoscopy, noted Dr. Margriet C. de Haan and Dr. Jaap Stoker from University Medical Center Amsterdam, and Dr. Steve Halligan from University College London.
"CTC enables visualization of the entire colorectum," they wrote. "Secondly, CTC has the advantage that it detects advanced neoplasia in an early phase. CTC screening results in a higher diagnostic yield per 100 invitees than primary gFOBT (guaiac fecal occult blood test), fecal DNA tests, and FIT (fecal immunochemical test) screening, and in a similar yield as sigmoidoscopy and colonoscopy screening," (European Radiology, 2 May 2012, online first).
CTC's ability to detect adenomas and cancers at an early stage makes the interval between tests -- 5-10 years -- much longer than stool tests, which must be repeated every two years, though only stool tests have demonstrated a mortality benefit to date. It can also detect abnormalities outside of the colon, a capability unique to CTC.
Based on aggregated results in studies of more than 4,000 participants, CT colonography showed an average per-patient sensitivity of 88% for lesions 10 mm and larger, including three studies demonstrating per-patient sensitivity for advanced neoplasia 6 mm and larger of 84% to 93%. A recent meta-analysis demonstrated sensitivity of 96% for lesions 10 mm and larger, comparable to that of colonoscopy, according to the authors.
This compares to lower sensitivity for commonly used stool tests gFOBT (11%-20%) and FIT tests (27-48 %), and equivalent numbers to CTC for conventional colonoscopy: 88% for all advanced neoplasia, they wrote. Sigmoidoscopy has a sensitivity of approximately 83% for advanced neoplasia and 58%-75% for cancers.
Participation matters a lot in screening programs as well -- and it has been highly variable in surveyed populations undergoing stool testing exams. A recent Dutch study showed that twice as many participants were invited to screen with either conventional or vertical colonoscopy, but considering its slightly lower sensitivity versus the invasive exam, the additional screening subjects put CTC on par with conventional colonoscopy in terms of diagnostic yield. A key reason may be that many patients prefer it to optical colonoscopy. Several comparative nonrandomized studies have shown CTC is less burdensome than colonoscopy, and an upcoming randomized study of 547 patients also favored virtual colonoscopy, although the randomized study was performed on a symptomatic cohort.
Recent studies have made the prep easier by using iodinated oral contrast instead of the traditional cathartic bowel preparation. "...noncathartic preparations are
increasingly popular and are expected to enhance compliance," the group wrote.
Finally, CTC has a better safety profile than optical colonoscopy, but the authors cautioned that the correct approach is to consider the diagnostic pathway as a whole, since patients who are positive still need to be referred for optical colonoscopy, where they face all of the risks of that exam.
The main disadvantage of CTC is the requirement for subsequent colonoscopy after any tests in which clinically significant lesions are detected. If the referrals are limited to lesions 10 mm and larger, studies in asymptomatic screening populations show referral rates of about 8-9%. However, if patients with polyps ≥ 6 mm are referred the referral rates can be twice as high, for example 16.7% in a recent Dutch trial.
Radiation exposure for CTC is a concern, the authors noted, but it may be overemphasized. Gonzales et al estimated CTC would prevent the development of 24 colorectal cancer cases for every radiation-induced cancer from CTC screening -- and that figure was calculated from per-exam exposure rates of 7-8 mSv, when in fact the average dose is closer to 4 mSv.
Cost-effectiveness is still somewhat an unexplored territory, but most cost-effectiveness analyses derived from data extracted from literature have found CTC by itself is not cost-effective at current unit costs of 346 to 594 euros ($444 to $760 U.S.), though costs are likely to be lower when applied strictly to asymptomatic screening patients.
"Ultimately, the key-metric required by health policymakers will be the cost-per-cancer detected and the cost-per-significant-adenoma detected per 100 subjects invited for screening, which allows direct cost-comparisons between competing screening modalities," de Haan et al wrote. "The costs, diagnoses, and consequences of screening should be collected prospectively as part of a randomized controlled trial (or established screening program) so that the cost-effectiveness model is populated with reliable data rather than test characteristics and costs estimated from the literature, which may be inaccurate or derived from healthcare settings that are not generalizable to the setting in question."
Before wide-scale implementation occurs, however, capacity will need to be expanded, meaning investment in more readers and facilities, and possibly including the training of radiographers to handle some aspects of interpretation.
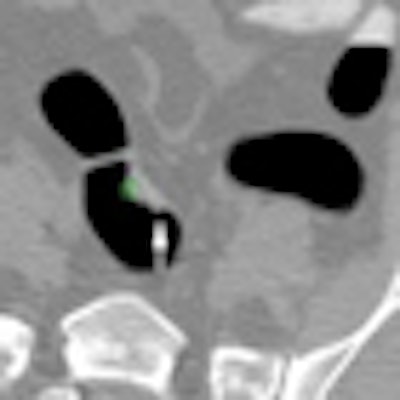
The increased use of computer-aided detection (CAD) could also improve capacity and accuracy, and has been shown to increase sensitivity significantly for lesions 6 mm and larger, the group wrote.
CAD might also be used as the primary CTC reader followed by a radiologist evaluation. An Italian study of FOBT positives recently showed that such a reading detected 11 of 13 colorectal carcinomas.
"If the evaluation of CAD findings was followed by evaluation of the 2D images, this resulted in a sensitivity of 89% for advanced adenomas, which was comparable to double primary 2D read followed by secondary CAD read," they noted.
As part of colorectal cancer screening programs in many European countries, CTC has supplanted barium enema as the preferred whole-colon examination in gFOBT-positive patients who cannot undergo colonoscopy or who have incomplete results at colonoscopy. Overall, studies show accurate lesion detection, and feasibility of the exam supporting the use of CTC for screening, but there's more to it than that, the authors concluded.
"The viability of CTC as a primary screening investigation is likely to turn on other factors, such as cost-effectiveness and whether the ability to detect extracolonic disease (impossible with alternative investigations) is ultimately beneficial or not," they wrote. "Whether there is a need to demonstrate a direct reduction in disease-specific mortality is debatable given that detection characteristics of CTC for cancers and adenomas are well-defined. However, the CTC community should be aware that the lack of large-scale implementation pilots, including an evaluation of effect on disease-specific mortality, remains an obstacle for health policymakers shaping population-based CTC screening in Europe in the future."















