3D elastography can be applied to an automated breast volume scanner to analyze in vivo strain images, according to a study published on December 15 in Ultrasound in Medicine & Biology.
Researchers led by Gijs Hendriks from Radboud University Medical Center found that strain elastography could differentiate between malignant and benign breast lesions when applied to the automated scanner, imaging these in three dimensions.
“The results indicate that maximal principal strain ratios were significantly increased in malignant lesions compared with benign lesions including fibro-adenoma,” Hendriks and colleagues wrote.
Automated breast volume scanners have been employed in recent years to overcome the inherent limitation of ultrasound, user dependability. While previous reports have highlighted the high sensitivity and fair inter-observer agreement from these scanners, they also indicated that the scanners suffer from low specificity. This leads to higher recall rates, more follow-up exams, and unnecessary biopsies.
Previous studies have demonstrated that adding 2D elastography to B-mode ultrasound improves specificity for malignant lesion detection. This is due to malignant lesions being stiffer with increased strain ratio compared to benign lesions. Still, this method is user-dependent.
The Hendriks team investigated whether adding 3D quasi-static elastography to an automated breast volume scanner could help differentiate between malignant and benign breast lesions.
The researchers collected volumetric breast ultrasound data from 82 women before and after automated transducer lifting. They annotated and calculated strain from elastography using an in-house algorithm. Additionally, they calculated two strain ratio types, axial and maximal principal strain.
The team reported 44 lesions detected. These included nine cancers, 23 cysts, and 12 other benign lesions.
Adding 3D elastography to the automated scanning protocol showed a significant difference between malignant and benign lesions. On maximal principal strain, the median strain ratio was 1.7 in malignant lesions, with a range between 1.0 and 3.2. Benign lesions meanwhile had a median strain ratio of 1.0, with a range between 0.6 and 1.9 (p = 0.007).
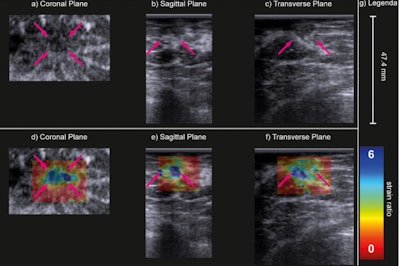 B-mode (a–c) and strain ratio (d–f) images of a carcinoma of unknown type in the coronal (a, d), sagittal (b, e) and transverse (c, f) planes. In the strain images (d–f), the maximal principal strain ratios are superimposed on the B-mode images of the top row. The purple arrows indicate the lesion. Image courtesy of Ultrasound in Medicine & Biology. Image available for fair use under creative commons license.
B-mode (a–c) and strain ratio (d–f) images of a carcinoma of unknown type in the coronal (a, d), sagittal (b, e) and transverse (c, f) planes. In the strain images (d–f), the maximal principal strain ratios are superimposed on the B-mode images of the top row. The purple arrows indicate the lesion. Image courtesy of Ultrasound in Medicine & Biology. Image available for fair use under creative commons license.
The team also found no significant difference in strain ratios between malignant and benign lesions when it came to using axial strain ratio. This included a median ratio of 0.8 for malignant lesions and 0.6 for benign lesions.
“Negative axial strain ratios indicated that the axial strain in the lesion was opposite in sign to that of the reference area,” the researchers added.
The next step is to test this imaging method in a larger population to further study breast density-strain dependency, as well as verifying its feasibility, the study authors wrote. They added that they eventually would like to study this method in a large screening population to evaluate clinical performance.
“Furthermore, the reproducibility and repeatability of the method have to be verified,” the authors added.
The full study can be found here.