Understanding the types of MRI artifacts in spinal imaging is vital for recognizing the limitations of the study and avoiding potential pitfalls, researchers from Australia have underlined.
"Artifacts can occur as a result of MRI hardware, scanning parameters or patient factors," said first author Dr. Mohammad Danish Mangi, from the Faculty of Health and Medical Sciences at the University of Adelaide. "Not only can this negatively affect the quality of the images, but it can also be confused with pathology."
MRI of the spine is used increasingly for indications such as back pain, radiculopathy, claudication, inflammatory arthropathy, trauma, and cancer staging, but interpretation can be complicated by the presence of artifacts. It's important to be able to recognize artifacts and potentially resolve them or use them to one's advantage, Mangi noted in a poster at the annual scientific meeting (ASM) of the Royal Australian and New Zealand College of Radiologists (RANZCR), held recently in Brisbane.
Chemical shift phenomenon
The chemical shift phenomenon is also known as "misregistration" or "mismapping," and it occurs due to the slower resonating frequency of protons in fat compared to water, resulting in a shift in signal intensity along the fat-water interfaces. This is more prominent with at higher magnetic field strength and narrower bandwidth, according to Mangi and his co-author Dr. WanYin Lim, a radiologist at Royal Adelaide Hospital and Jones Radiology.
"In MRI of the spine, this can be seen as alternating bright and dark outlines at the sides of vertebral bodies," they explained. "These artifacts can also be seen around lipomatous and cystic lesions in the spine, such as a lipoma."
These may mimic disc bulge and can exaggerate foraminal narrowing as the discovertebral junction is a fat-water interface. The India ink artifact is a type of chemical shift phenomenon seen on gradient echo sequences. It manifests as a black boundary at the fat-water interface.
Chemical shift artifact can be eliminated by using a fat-suppressed sequences. A smaller field of view and wider bandwidth can also reduce this artifact, but this comes at the cost of image resolution, the authors pointed out.
Artifacts due to motion
Motion artifacts can occur due to the patient changing position during scan acquisition. In addition, "ghost" artifacts can occur from periodic motion such as blood flow, cerebrospinal fluid (CSF) pulsation, and swallowing.
"Artifacts due to patient movement occur in the phase-encoding direction as this step usually take the longest and is acquired line by line, and can lead to blurring or ghosting of structures," the researchers stated. "The signal of the structure is displayed over its range of motion, resulting in blurring and decreased edge definition. The study may be rendered nondiagnostic."
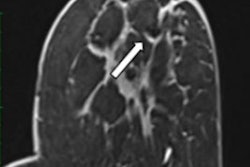
Artifacts due to CSF pulsation are more often seen in the cervical and thoracic spine compared to the lumbar spine. These artifacts appear as signal heterogeneity within the thecal sac voids, with focal areas of signal loss in the CSF.
"This can be mistaken for a dural arteriovenous fistula, although the latter has a characteristic serpiginous appearance," they noted. "This is a useful artifact as its absence in the context of spinal cord deviation can indicate an arachnoid cyst."
If there is cord deviation with preserved CSF pulsation artifact, ventral dural herniation or arachnoid web will be more likely, the authors continued.
Artifacts due to swallowing or similar movements involving the cervical spine can cause a series of ghost images that can obscure the spinal cord and possibly diminish its size. Repeating the study and applying a presaturation pulse will reduce this artifact.
Artifacts due to non-uniform magnetic field
Failure of fat suppression artifacts commonly occur. Frequency-selective presaturation is the most common method of eliminating unwanted signal from fat. Inhomogeneity in the static magnetic field can cause this to fail, usually occurring when there is a large field of view, the authors wrote.
In this situation, the fat in vertebrae may not be suppressed at the edge of the scan field, leading to abnormal bright signal in areas where fat should have been saturated and fat signal nulled. In this area, water may be saturated instead of fat, causing signal loss from the spinal cord which can simulate or obscure pathology, they continued.
"This artifact is particularly severe at the back of the neck, especially at the cervicothoracic junction, due to the geometry of the fat-air interface at this site," they noted.
Metallic susceptibility artifacts usually present as a signal void associated with peripheral signal hyperintensity. Ferromagnetic artifact is greater with gradient echo imaging than it is with both conventional and fast spin echo imaging. It is worse with reduced bandwidth, large voxel sizes, and high-field strength magnets.
"Nonmagnetic stainless steel can also cause artifacts on MRI because the material has residual paramagnetic properties. Titanium implants are associated with less surrounding tissue distortion artifacts compared to stainless steel," the researchers wrote.
Artifacts due to scanning parameters
The shading artifact is due to a nonuniform radiofrequency field produced by a surface coil, and this causes the signal intensity of the image to be uneven, with loss of signal intensity in parts of the image further from the surface coil. Saturation artifact (cross talk/coherence) may occur when angled axial images of the lumbar spine are obtained simultaneously. A band of signal loss will be present where they overlap due to signal interference, they added.
Wraparound artifact (aliasing) results when signal from tissue outside the field-of-view is mapped. The signal received is misplaced onto the opposite side of the image. This can potentially obscure lesions of the spine and adjacent tissues.
Truncation artifact (Gibbs Phenomenon) occurs due to the inability of Fourier transformation to reproduce signal intensity changes at high contrast interfaces accurately, for example at the discovertebral junction and CSF-cord interface.
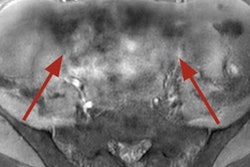
The dielectric effect is seen when using higher magnetic field strengths, typically 3T or more, and occurs when the radiofrequency wavelength is of similar magnitude or smaller than the patient's cross-sectional diameter, leading to constructive and destructive interference patterns and hence, areas of increased or decreased signal intensity.
At a field strength of 3T, the radiofrequency wavelength is 26 cm, which may be smaller than the abdominal diameter, particularly in patients with obesity, ascites, or pregnancy. "Central decreased intensity can obscure pathology," they concluded.
Editor's note: You can view the whole poster on the EPOS section for the RANZCR ASM 2023 on the ESR's website.