Ten years have passed since gadolinium (Gd) retention -- or deposition -- in the brain was first described. To mark the anniversary, European MRI experts have reflected on the current state of knowledge of Gd retention and deposition resulting from the use of linear gadolinium-based contrast agents (GBCAs).
"After 10 years, even though there is evidence that GBCAs are retained and that sometimes Gd is deposited in tissues, there is no evidence of clinical symptoms nor harm associated with Gd deposition in the brain and body," Dr. Aart van der Molen, a radiologist at Leiden University Medical Center in the Netherlands, and colleagues noted in an article posted on 7 October by European Radiology.
There are still many knowledge gaps about Gd metabolism and Gd deposition for which an international research agenda is important, stated the authors, who are members of the European Society of Magnetic Resonance in Medicine and Biology Gadolinium Research and Educational Committee (ESMRMB-GREC). They said they keenly await the results of ongoing studies issued by the Federal Drug Authority on the joint contrast media manufacturers.
Back to basics
A basic understanding of GBCA physicochemistry, transmetallation, and elimination is vital to understand Gd retention, they emphasized.
GBCA exploits the highly paramagnetic gadolinium, which shortens T1 and T2 of tissues, leading to increased signal intensity (SI) on T1-weighted (T1w) images and reduced SI on T2-weighted images.
After intravenous administration, extracellular GBCA is excreted by the kidneys with an early elimination half-life of more than two hours in patients with normal renal function, while over 95% of the GBCA is cleared from the body within 12 hours; both are similar for linear and macrocyclic GBCA.
"Hepatobiliary GBCA has additional intracellular transient uptake and hepatic excretion into the biliary tree. In patients with severely reduced renal function (estimated glomerular filtration rate < 30 ml/min/1.73 square meter), this early elimination half-life can increase up to 30h, which can increase the likelihood of transmetallation," the authors explained.
A review of pharmacokinetic data showed the presence of a deep compartment of distribution with long-lasting residual excretion, they added. "So far, the exact components of this deep compartment are unknown. This long-lasting excretion is faster for macrocyclic GBCA and is correlated to the higher thermodynamic stability and differences in transmetallation."
Frenzy of studies
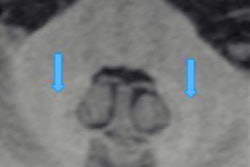
In 2014, visible hyperintensities on unenhanced T1w images in the nucleus dentatus and globus pallidus of the brain were associated with previous GBCA injections and gadolinium deposition in patients with normal renal function. This led to a "frenzy of retrospective studies with varying methodologies," according to van der Molen and colleagues.
"It was suggested that the retrospectively observed hyperintensity of the dentate nucleus and the globus pallidus relative to the pons (i.e., dentate nucleus to pons ratio) on unenhanced T1w images of a population of patients with brain tumours was related to repeated administrations of linear GBCA," they noted. "Almost simultaneously, a European group reported similar findings on unenhanced T1w brain images after multiple injections of gadodiamide in patients with multiple sclerosis and in patients with brain metastases."
It is unclear what forms are responsible for the T1w signal increase, they continued.
"In the rat brain, three different chemical forms must be distinguished: intact GBCA, Gd bound to macromolecules (e.g., ferritin), and insoluble Gd-salts," the authors explained. "Intact GBCA was found for linear and macrocyclic GBCA, but the other forms were only for linear GBCA. As precipitated gadolinium does not induce any change in MRI signal, it is likely that the Gd bound to macromolecules is responsible for the visible T1w hyperintensity in clinical MRI.
Gd retention in the body
Most of the data regarding the abdominal organs is still largely investigational and no firm conclusions can be drawn yet. There is a paucity of data from human studies. Reduced T1 values in the renal cortex and medulla have been demonstrated after seven days of a single dose of gadobutrol in subjects with normal renal function using T1 mapping. This indicates the prolonged presence of small amounts of gadobutrol in the kidney after single-dose administration, suggesting delayed elimination of GBCA.
Gd deposits have been associated with iron overload in the livers of pediatric stem cell transplantation patients with normal renal function, the authors noted.
Possible clinical symptoms
Despite the retention or even deposition of Gd in various tissues, no histopathologic changes in rat brains could be found, nor tissue alterations in multiple sclerosis (MS) patients, they wrote. In addition, no effect on sensorimotor or behavioral functions could be demonstrated for either linear or macrocyclic GBCAs in mice or in humans. Gadolinium retention was not related to symptom worsening in relapsing MS patients nor to Parkinsonism.
For linear GBCAs, pain hypersensitivity has been seen in rats. In MS, increased relaxation rates may be associated with lower information-processing speed or mild effects on cerebellar speech or verbal fluency, but these couldn't be fully attributed to GBCAs, according to van der Molen and colleagues.
"Dermal thickening of the scalp skin has been reported in MS patients with normal renal function exposed to linear GBCA as compared to a matched group of patients exposed to macrocyclic GBCA, thus suggesting subclinical chronic effects of gadolinium retention on the skin," they noted.
In clinical practice, radiologists need to minimize Gd deposition ensure a strict indication for contrast-enhanced MRI and only use European Medicines Agency-approved or American College of Radiology (ACR) grade II GBCA in all patients.
The ACR/National Institutes of Health/RSNA Agenda remains a good guidance document to target future research, the authors pointed out.
You can read the full European Radiology article here.